An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


ADHD: Reviewing the Causes and Evaluating Solutions
Luis núñez-jaramillo, andrea herrera-solís, wendy verónica herrera-morales.
- Author information
- Article notes
- Copyright and License information
Correspondence: [email protected] ; Tel.: +52-983-8350300 (ext. 241)
Received 2020 Dec 31; Accepted 2021 Feb 23; Collection date 2021 Mar.
Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/ ).
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder in which patients present inattention, hyperactivity, and impulsivity. The etiology of this condition is diverse, including environmental factors and the presence of variants of some genes. However, a great diversity exists among patients regarding the presence of these ADHD-associated factors. Moreover, there are variations in the reported neurophysiological correlates of ADHD. ADHD is often treated pharmacologically, producing an improvement in symptomatology, albeit there are patients who are refractory to the main pharmacological treatments or present side effects to these drugs, highlighting the importance of developing other therapeutic options. Different non-pharmacological treatments are in this review addressed, finding diverse results regarding efficacy. Altogether, ADHD is associated with different etiologies, all of them producing changes in brain development, leading to the characteristic symptomatology of this condition. Given the heterogeneous etiology of ADHD, discussion is presented about the convenience of personalizing ADHD treatment, whether pharmacological or non-pharmacological, to reach an optimum effect in the majority of patients. Approaches to personalizing both pharmacological therapy and neurofeedback are presented.
Keywords: ADHD, heterogeneous etiology, pharmacological treatment, neurofeedback, qEEG informed neurofeedback, treatment personalization
1. Introduction
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder (NDD) presenting with inattention, hyperactivity, and impulsivity. It can be classified in three subtypes, depending on the intensity of the symptoms: predominantly inattentive, predominantly hyperactive–impulsive, and combined [ 1 , 2 ]. ADHD has a global prevalence of 5.9% to 7.1% in children and 1.2% to 7.3% in adults [ 3 ].
While most studies address ADHD in children from 7 to 17 years old, it is important to outline that this condition is also present in adults. It has been proposed that the number of adults with ADHD has increased over the last 20 years. A part of this increase is due to the permanence of ADHD symptoms in the adult age in 76% of diagnosed patients. ADHD implies important challenges for academic, personal, and job performance [ 4 ].
As for any other condition affecting brain function, in order to find an adequate treatment for ADHD, it is important to first understand its physiological basis. As with other NDDs, the causes of ADHD are aberrant neural development, affecting neurogenesis, synaptogenesis, myelination, and neuronal and glial proliferation and migration. Even though symptoms begin to appear in childhood, neuronal development is affected from early embryogenesis [ 5 ].
The etiology of ADHD is diverse—gestational, perinatal, and genetic factors have been associated with ADHD incidence. However, each patient presents only a few of them.
2. Environmental Factors Associated with ADHD
The incidence of ADHD is associated with a number of environmental factors during different stages of central nervous system (CNS) development, such as gestational and perinatal periods. In this section, we will address some of the environmental factors that have been associated with ADHD.
2.1. Preconceptional, Gestational, and Perinatal Conditions
Premature birth is an important risk factor for ADHD, since it has been reported that it occurs 2.6 to 4 times more frequently in babies born with low weight or very low weight. Premature birth is associated with alterations in neurogenesis and cell death [ 6 ], and these are in turn associated with reduced cortical expansion, as reported in ADHD patients [ 7 ]. One possible reason for increased risk of developing ADHD in preterm children is inflammation; an increase in inflammation-related molecules is associated with increased risk of developing ADHD symptoms [ 8 ].
Perinatal hypoxia is an environmental factor that increases the risk of developing AHDH, probably due to its effects on dopaminergic transmission and neurotropic signaling [ 9 ].
The intake of nutrients during gestation is very important for proper brain development. An important element during neural development is the polyunsaturated fatty acid docosahexaenoic acid (DHA), promoting proliferation and neural differentiation of neural progenitor cells. Decreased levels of DHA during brain development have been associated with ADHD and other neurodevelopmental disorders [ 10 ], and decreased levels of serum DHA levels have been reported in adult ADHD patients [ 11 ]. Additionally, malnutrition or immune activation in the pregnant mother is a risk factor for ADHD and other neurodevelopmental disorders [ 12 ]. High sucrose consumption during pregnancy is possibly related with ADHD incidence. A study performed on rats reported that high sucrose intake in pregnant rats led to the appearance of ADHD-like symptoms in the offspring, who showed increased locomotor activity, decreased attention, and increased impulsivity. Furthermore, the offspring also presented increased dopamine transporter (DAT) and a decrease in dopamine receptors and mRNA expression in the striatum [ 13 ].
Interestingly, there is evidence in a rat model of the influence of preconceptional conditions on ADHD incidence. Offspring of Female rats administered with ethanol for 8 weeks before mating presented ADHD-like symptoms such as hyperlocomotive activity, impulsivity, and attention deficit. These rats also presented low levels of striatal DAT and increased presence of norepinephrine transporter (NET) in the frontal cortex [ 14 ]. A later work by this group revealed that paternal preconceptional alcohol exposure also produced ADHD-like symptoms in the offspring, presenting decreased expression of DAT mRNA and DAT protein in the cortex and striatum. Furthermore, authors report epigenetic changes in both the sperm of these alcohol-exposed male rats and in the frontal cortex and striatum of the offspring, presenting increased methylation in a CpG region of DAT gene promoter, which is in agreement with the reduced expression of DAT in the offspring [ 15 ].
Another environmental factor associated with ADHD is pesticide exposure during development. A study addressing the issue, both at experimental and epidemiological levels, reported that exposure to the pesticide deltamethrin during gestation and lactation in rats led to ADHD-like symptoms, such as working memory and attention deficits, hyperactivity, and impulsive-like behavior. It also produced increased presence of DAT and D1 receptor in the striatum, as well as increased dopamine release and increased presence of D1 dopamine receptor in the nucleus accumbens. Interestingly, the authors also performed an epidemiological study in humans, revealing that children (6 to 15 years old) with detectable levels of pyrethroid metabolites in urine had more than twice the probability of being diagnosed with ADHD [ 16 ].
2.2. Heavy Metal Exposure
One of the most reported environmental factors associated with ADHD is exposure to neurotoxic heavy metals. A study performed on school children revealed that children (6–7 years old) with ADHD presented higher levels of salivary mercury. However, when including all age groups studied (12–13 years and 15–16 years), no significant correlation was found between increased salivary mercury and ADHD, although a mild tendency was observed [ 17 ].
In the case of manganese, both too high and too low blood levels are associated with cognitive deficits. High concentration of manganese in blood is associated with deficits in thinking, reading, and calculations, as well as with lower learning quotient (indicative of learning disability) and more errors in the continuous performance test (measuring attention and response inhibition). Conversely, low blood level of manganese is associated with a poorer performance in the Stroop test, which is used to assess cognitive inhibition [ 18 ]. Similarly, a study addressing the relationship between manganese in drinking water and ADHD found a higher risk of developing this condition (inattentive but not combined subtype) as exposure to manganese in drinking water increased [ 19 ]. However, a study on manganese in children’s deciduous teeth failed to find an association between this metal and cognitive deficits [ 20 ].
The presence of lead in children’s deciduous teeth is positively associated with hyperactivity or impulsivity, as well as inattention and oppositional or defiant disorder [ 20 ]. A study on children from a lead-contaminated region reported that blood levels of cadmium, lead, and manganese correlated with conduct problems and antisocial behavior [ 21 ]. Another work found a higher concentration of blood lead in ADHD children, which was correlated with hyperactivity–impulsivity symptoms but not with inattention [ 22 , 23 ]. Both genetic [ 24 ] and epigenetic [ 25 ] factors have been reported to contribute to lead-related pathogenesis of ADHD. Moreover, a study carried out in Argentina found that children with high blood concentrations of lead are more likely to develop ADHD [ 26 ].
A review on the effects of prenatal and childhood metal exposure on cognition found suggestive evidence of a relation between cadmium exposure and impaired cognitive ability in children. They did not find evidence of a relationship between cadmium exposure and ADHD [ 27 ]. A more recent study addressing cadmium exposure during pregnancy revealed that a higher blood cadmium concentration during pregnancy is associated with higher scores in ADHD diagnostic tests in female children at 6 years of age, but not in the case of male children [ 28 ].
A recently published work reported that ADHD children present higher urine concentrations of chromium, manganese, cobalt, nickel, copper, molybdenum, tin, barium, and lead [ 29 ]. A recent study analyzing serum concentrations of different metals in ADHD children reported low levels of chromium, manganese, and zinc, as well as increased copper/zinc ratios in these children [ 30 ]. A meta-analysis on the relation between blood and hair zinc and ADHD found no statistical difference between ADHD and control children [ 31 ].
Thus, there are a number of environmental factors associated with ADHD incidence. While environmental factors are not found in all ADHD cases, the data reviewed herein highlight the importance of environment in different developmental stages—and even before conception—in regard to the risk of developing ADHD.
3. Sleep Disorders and ADHD
Sleep deprivation, either acute or chronic, produces decreased cognitive functioning (one of the main traits of ADHD). Interestingly, it also produces the externalizing symptoms observed in ADHD patients. For example, a very tired child might become hyperactive, while in a sleepy adult in a condition where it is not possible to sleep (for example, while driving), the externalizing behavior will help them to remain awake. Thus, both of the core ADHD symptoms can be produced by sleep deprivation. Conversely, hyperactivity in children or high internal activity in adults in the evening might lead to sleep disruption [ 32 ].
Among the sleep disorders found in ADHD patients are delayed sleep phase disorders, insomnia, sleep-disordered breathing, increased motor activity during the night, sleep anxiety, clenching teeth, periodic limb movement, restless legs, increased sleep onset latency and shorter sleep time, night awakenings, narcolepsy, and parasomnias [ 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ]. Among them, delayed sleep phase disorder is one of the most frequently found, being present in 73–78% of both ADHD children and adults. This condition consists of a delay between the sleep propensity cycle and the circadian cycle, leading to increased daytime sleepiness and decreased cognitive functioning [ 32 ].
Sleep disturbance have an impact on daytime vigilance, producing excessive sleepiness [ 32 , 37 , 39 ], and can exacerbate inattention, impulsivity, and hyperactivity as means to remain awake [ 32 , 37 ]. Additionally, stimulant medication might also cause sleep disturbances, although OROS methylphenidate produces less adverse effects on sleep [ 34 , 36 ]. LDX, a stimulant prodrug that undergoes hydrolysis in the bloodstream releasing d-amphetamine, and atomoxetine, a non-stimulant pharmacological treatment for ADHD, do not produce adverse effects on sleep [ 36 ].
Sleep disturbances in ADHD patients can produce significant impairments in attention, mood, and behavior [ 32 , 35 ]. Physiologically, there is evidence supporting an overlap between brain centers regulating sleep and those regulating attention and arousal, so it is possible that affectation of one of these systems also affects the other. Similarly, affectation of noradrenergic and dopaminergic pathways is found in both ADHD and sleep disturbances [ 40 ].
Conversely, during wake time, sleep disturbances produces symptoms resembling those observed in ADHD patients [ 35 , 41 , 42 ]. It is, thus, recommended to assess sleep disorders in patients with ADHD symptoms in order to avoid misdiagnosis [ 41 , 42 ].
The relationship between sleep disorders and ADHD is complex. While ADHD might produce sleep disorders, they could also be coincident conditions [ 36 ]. Moreover, sleep disorders have been proposed to be not only one of the intrinsic features of ADHD, but also might be one of its causes [ 32 , 36 ]. Another possible explanation for this interaction would be an underlying common neurological disease leading to both sleep disorders ad ADHD [ 36 ]. A recent review on the subject proposed that chronic sleep disorders are some of the main causes of ADHD symptoms [ 32 ]. The authors suggested that patients presenting ADHD symptoms should undergo quantification of sleep and sleep problems in order to rule them out as the sole cause of ADHD symptoms. Thus, ADHD treatment should address both the symptoms (with classic ADHD treatment) and the sleep problem [ 32 , 34 , 35 , 36 ], although the effect of this combined treatment still requires further research [ 32 ].
4. Genetic Factors Associated with ADHD
Different studies have revealed an important genetic influence in the etiology of ADHD [ 43 ]. It is a polygenic condition with an important number of genes involved, as confirmed by a genome-wide association study on ADHD reporting 12 significant loci associated with this condition [ 44 ]. Many of the genes reported to be associated with ADHD participate in processes such as neurotransmission, neuritogenesis, synaptogenesis, or receptor location in synapses [ 45 ]. In this review, we will focus on two genes, a neurotrophin (brain-derived neurotrophic factor –BDNF-) and a molecule involved in dopaminergic signaling (DAT).
Brain-derived neurotrophic factor (BDNF) is a neurotrophin with high expression in the brain that is highly concentrated in the hippocampus and cortex. It has an important role in neuronal development, being important for neuronal proliferation, migration, differentiation, and maturation, as well as for synaptogenesis [ 46 ].
BDNF has been implied in ADHD pathophysiology. It has been proposed that low levels of this neurotrophin may explain the reduction in brain volume observed in ADHD patients, and it has also been implied in dopaminergic system homeostasis. Some pharmacological treatments for ADHD promote the regulation of plasma BDNF levels [ 47 ].
4.1.1. Circulating BDNF
Since BDNF is able to cross the blood–brain barrier and plasma concentrations of BDNF are highly correlated with its levels on cerebrospinal fluid, a number of studies have searched for a difference in plasma concentrations of BDNF in ADHD patients when compared against controls. There are reports indicating a lower concentration of BDNF in plasma of ADHD patients, both in children [ 48 ] and adults [ 49 ]. In another study involving children, an increase in plasma BDNF was observed after 6 weeks of treatment with an effective dose of methylphenidate [ 50 ]. In accordance, a recent study revealed that methylphenidate treatment produces an increase in serum BDNF in boys with ADHD [ 51 ]. However, this has not always been replicated, since there are also articles reporting no difference in serum BDNF between children with ADHD and controls [ 52 , 53 , 54 ].
A recently published meta-analysis encompassing studies comparing BDNF levels in ADHD patients without any other comorbidity found no overall difference between ADHD patients and controls. However, when analyzing males and females separately, they found significantly higher levels of plasma BDNF in males with AHDH than in control males, while no difference was found between females with and without ADHD [ 55 ].
Thus, different and even contrary results have been obtained regarding BDNF concentrations in plasma or sera of ADHD patients. While this suggests that the link between BDNF and ADHD is not completely clear, other alternatives should be considered. For example, fluctuations in serum BDNF concentrations in morning and evening samples have been reported [ 56 ], meaning the lack of relation between peripheral BDNF concentration and ADHD might be due to the time of the day when the sample was obtained.
4.1.2. Genetics of BDNF
There are a number single nucleotide polymorphisms (SNP) of the BDNF gene that have been associated with ADHD. Among the most studied variations in the BDNF gene, there is a polymorphism called Val66Met (also known as rs6265), in which a change in codon 66 produces a substitution of the original amino acid (valine) by methionine. The anatomical effects of this variation are more apparent in the hippocampus and cortex [ 46 ]. While some studies have assessed the presence of this SNP in ADHD patients [ 57 , 58 , 59 ], other studies failed to find an association between this polymorphism and ADHD [ 46 , 60 , 61 , 62 , 63 ].
Another SNP of the BDNF gene whose association with ADHD is not conclusive is rs2030324, since some studies report an association between this polymorphism and ADHD [ 57 , 58 , 59 , 64 ], while other reports fail to find this association [ 46 , 60 , 61 , 62 , 63 ].
There are other SNPs of the BDNF gene that have been studied so far, with positive correlations being shown between ADHD and the presence of C270T (rs27656701) [ 58 , 61 ], rs11030101 [ 62 , 64 , 65 ], and rs10835210 [ 62 , 63 ]. There are also reports addressing SNPs of the BDNF gene for which no association with ADHD has been found, including rs12291186, rs7103411 [ 63 ], and rs7103873 [ 62 , 63 ].
Moreover, rare single nucleotide variants of BDNF gen have also been associated with a higher risk of developing ADHD [ 66 ]. However, this is an area that requires further research.
As observed with peripheral BDNF concentrations, genetic variants of the BDNF gene have been associated with ADHD in numerous cases, although in some cases there are contradictory results in different articles (see Table 1 ). Moreover, some of the genetic variants of the BDNF gene associated with ADHD have also been studied in association with other neurological conditions and treatments. For example, C270T is reported to be associated with intellectual disabilities [ 58 ]. Moreover, rs11030101 is associated with a better response to electroconvulsive shock therapy for treatment-resistant depression [ 67 ], with body weight gain in schizophrenic patients treated with atypical antipsychotics [ 68 ], as well as with the presence of major depressive disorder [ 69 ], schizophrenia, and bipolar disorder [ 70 ], although there is another publication in which no evidence of association between this SNP and bipolar disorder was found [ 71 ]. Additionally, rs10835210 has been associated with bipolar disorder, schizophrenia [ 70 ], and phobic disorders [ 72 ].
Polymorphisms of the BDNF gene studied in relation with ADHD incidence. * Polymorphisms for which contradictory results have been reported. rs, reference SNP ID number.
For rs6265 (Val66Met), there are many articles addressing the association of this SNP with different conditions, and in some of them it has been found. For example, some articles report an association of this SNP with major depressive disorder [ 69 , 73 ], while other studies fail to find this association [ 74 , 75 ]. An association has also been reported between rs6265 and amnestic mild cognitive impairment, as well as with the transition from this condition to Alzheimer’s disease [ 76 ]. However, in patients with early-stage breast cancer, this SNP is associated with a lower probability of presenting cognitive impairment after chemotherapy [ 77 ].
4.1.3. Other Neurotrophines
While BDNF has been widely studied in association with ADHD, it is not the only neurotrophin studied in relation with this condition, given the important role of neurotrophines in central nervous system development and synaptic plasticity. In this regard, there are studies addressing the participation of fibroblast growth factor (FGF), vascular endothelial growth factor, insulin-like growth factor (IGF2) [ 47 ], glial-derived neurotrophic factor (GDNF), nerve growth factor (NGF), and neurotrophin-3 (NTF-3) [ 47 , 53 ] in ADHD pathophysiology.
BDNF is a molecule highly involved in synaptic plasticity and has an undisputed role in central nervous system development. Therefore, it is not surprising to find a number of studies associating alterations in the presence of this neurotrophin in serum, or different SNPs of its gene, with ADHD. However, its role in ADHD development is not a constant for every sample of ADHD patients studied so far, and for many of the aspects of this molecule (serum levels, SNPs) there are reports indicating associations, with others finding no association at all. This does not mean that the alterations associated with this molecule are not important for ADHD, but rather highlight the variable etiology of this condition.
4.2. Dopaminergic System
The dopaminergic system emerges in early stages of CNS embryonic development, and an imbalance in this system might affect brain development. It is related with cell proliferation, neuronal differentiation and migration, synaptogenesis, and neurogenesis. Thus, it is not surprising that a role of this neurotransmitter system has been reported in different neurological diseases, including ADHD [ 78 ].
One of the most studied molecules of the dopaminergic system in relation to ADHD is DAT, a molecule responsible for dopamine reuptake, and the main target of two commonly used pharmacological treatments for ADHD, methylphenidate and amphetamines [ 78 ]. Genetic studies support the importance of this neurotransmission system for ADHD. Mice heterozygous for the DAT gene (+/− heterozygotes) are reported to present altered attentional function [ 79 , 80 ] and hyperactivity [ 80 ], while rat models with this heterozygous genotype do not present major affectations [ 81 , 82 ]. However, DAT knockout rats present hyperactivity [ 81 , 82 ], as well as a dysregulation in frontostriatal BDNF function [ 82 ]. Hyperactivity in these rats can be counteracted by amphetamine, haloperidol, and methylphenidate [ 82 ].
In humans, ADHD patients present lower DAT availability in the basal ganglia, caudate nucleus, and putamen [ 83 ]. The DAT gene presents a variable tandem repeat region (VNTR) at the untranslated 3′region, and there are different alleles for this VNTR, with the 9-repeat and 10-repeat alleles being the most frequently encountered. The reported effects of this VNTR on DAT expression vary in different articles, however the most recent results indicate that the 9-repeat allele is associated with a higher DAT expression than the 10-repeat allele. [ 84 ]. The possible association between this VNTR and ADHD has been addressed in various studies. For example, an analysis of both patients and the literature found an association of the 10-repeat/10-repeat genotype with ADHD only in adolescents [ 85 ], studies performed in children reported an association between the 10-repeat/10-repeat genotype and ADHD [ 86 , 87 ], while a recently published meta-analysis reported an association of the 10-repeat allele with ADHD in children and adolescents, specifically in European population [ 88 ]. However, there are also reports indicating no association at all between ADHD and the VNTR of DAT gene (9-repeat/10-repeat, 10-repeat/10-repeat, and 10-repeat/11-repeat genotypes) [ 89 ], no association between the 10-repeat/10-repeat allele with ADHD [ 90 ], and no association between ADHD and the 9-repeat or the 10-repeat alleles for this polymorphism [ 91 ]. The last three studies were performed in children.
Additionally, the relevance of this VNTR has been studied in relation to cognitive function in healthy subjects. Again, mixed results were found. A meta-analysis published in 2016 addressing studies performed in healthy subjects did not find any association between DAT VNTR and different cognitive functions, such as executive functions, inhibition, attention, and long-term declarative memory [ 92 ]. A study performed in children aged 3 to 5 years old addressing the presence of the 9-repeats and 10-repeats alleles revealed that the presence of the 10-repeat allele of the DAT gene is associated with diminished ability to voluntarily regulate reactivity in healthy children [ 93 ]. A recent study on both ADHD and healthy children reported an effect of the specific genotype in the performance of children on attentional switching when studying the whole research sample, in which children carrying the 9-repeat allele performed worse than those carrying the 10-reapet homozygous or the 10-repeat/11-repeat heterozygous allele [ 91 ]
The participation of the dopaminergic system in the pathophysiology of ADHD has been widely reported [ 78 ]. Herein, we study a particular variation of the DAT gene, a VNTR in the 3′ region of the gene, finding articles supporting a role of this polymorphism in ADHD, as well as works failing to find an association between this VNTR and ADHD. This does not imply a lack of importance of this variation, but rather highlights the variability in the genetic etiology of this condition. Moreover, while the dopaminergic system is highly involved in the pathophysiology of ADHD, given its role in CNS development, it is also strongly related with other neuropsychiatric conditions, such as autism [ 78 , 94 , 95 ] and schizophrenia [ 78 , 94 , 96 , 97 ].
5. Changes in Brain Structure and Function in ADHD Patients
As an NDD, ADHD involves alterations of mechanisms such as neurogenesis and synaptogenesis. There are a number of possible mechanisms through which these alterations take place, both environmental and genetic, some of which have been mentioned in the present review. In the end, all of these altered mechanisms produce an altered brain function affecting attention and impulse control, functions regulated by the central nervous system. Understanding the changes in brain function associated with ADHD might shed some light not only on the functional causes of this condition, but also on possible ways to deal with it.
5.1. Brain Imaging Studies
Children with ADHD present atypical connectivity in reward circuitry when compared with control children. Increased connectivity of the nucleus accumbens with the prefrontal cortex was observed to be associated with greater impulsivity [ 98 ].
Hypofunction and abnormal cortico-striatal pathways of the cortico-striato-thalamo-cortical (CSTC) circuit are associated with ADHD. Five different CSTC circuits have been reported: the sustained attention circuit, emotion circuit, selective attention circuit, hyperactivity circuit, and impulsivity–compulsivity circuit. Four of them (except emotion circuit) have been related with ADHD diagnostic criteria. However, pathogenesis of the emotion circuit is also related with ADHD [ 99 ]
A study on ADHD children reported significantly decreased white matter volume, as well as decreased volume in the cortex and caudate nucleus, although it did not reach statistical significance. Cortical thickness was reduced in ADHD patients bilaterally in the frontal cortex and in the right cingulate cortex, structures related with executive function and attention. Regarding default mode network, functional connectivity was reduced in ADHD children in the anterior and posterior cingulate cortexes, lateral prefrontal cortex, left precuneus, and thalamus. However, connectivity was increased in the bilateral posterior medial frontal cortex [ 100 ].
A study on male adolescents with ADHD and controls reported decreased gray matter volume in the left anterior cingulate cortex and bilateral decreases in the occipital cortex, hippocampus–amygdala complex, and cerebellum in ADHD adolescents [ 101 ]. Such decreases in cerebellar volume have been previously reported in both female and male ADHD patients [ 102 ].
An important issue with many of the imaging studies in ADHD patients has been small sample size. A large-scale study performed on children, adolescents, and adults with ADHD reported decreased surface area in children, mainly in the frontal, cingulate, and temporal regions. This effect was more pronounced in younger children (4–9 years old). Moreover, cortical thickness in ADHD children is also reduced in the fusiform gyrus and temporal lobe, an effect more prominent in children of 10 and 11 years old. No change in surface area or cortical thickness was observed in adolescent or adult ADHD patients [ 103 ].
There are important changes in brain morphology in ADHD patients. An elegant study performed in ADHD patients and controls from 6 to 28 years of age analyzed differences in neurodevelopmental trajectories. This study reported that ADHD patients present overall reduced cortical volume, mainly in frontal lobes, and primarily due to a decrease in surface area and gyrification. Interestingly, although both groups presented maturational changes due to age, they presented different trajectories for these changes, suggesting that ADHD is associated with developmentally persistent changes in the whole cortex, mostly due to decreased surface expansion (reduced surface area and less convolution) [ 7 ].
When comparing children with comorbid epilepsy and ADHD with control children, a widespread decrease in cortical thickness is observed, along with decreased volume in some subcortical structures and the brainstem. These alterations were observed early in the course of epilepsy, thus the authors suggested that neurodevelopmental changes occurred before epilepsy onset [ 104 ]. In children with comorbid autism spectrum disorder and ADHD, when compared with typically developing controls, presented significantly lower volumes in left postcentral gyrus. This was observed through magnetic resonance imaging in both children and preadolescents, but was absent in adolescents. The authors suggested that pathophysiology in these comorbid patients may be related to somatosensory deficits and delayed maturation in this area [ 105 ].
5.2. Quantitative Electroencephalography
All these changes lead to alterations in brain function. A frequently used technique for the study of brain activity is quantitative electroencephalography (qEEG), since it has a low cost, a high temporal resolution, and does not need special facilities to be performed. Furthermore, qEEG has also been used to determine the effects of pharmacological treatments on brain activity in order to assess effectiveness [ 106 , 107 ], to choose the correct pharmacological option for a patient [ 108 ], to study the effects of previous pharmacological treatments on the current one [ 109 , 110 ], as well as to determine a possible cognitive effect of the chosen pharmacological treatment [ 111 ].
During the last decades, several studies have performed qEEG analyses on ADHD patients. A review on the subject published in 2012 addressed the main associations between brain activity and ADHD, including increased frontocentral theta activity. Another frequently reported factor, although not always replicated, is an increased theta/beta ratio. For beta and alpha bands, most of the reports have indicated decreased activity, although there are also reports that have indicated increased activity in these frequency bands in ADHD patients [ 112 ]. One of the most used indicators for ADHD is the theta/beta ratio in the Cz region. It has been reported that ADHD children (inattentive and combined subtypes) present increased theta/beta ratios [ 1 ]. Another study found that children with ADHD presented more delta and theta activity [ 113 ]. However, some authors have mentioned that this measure is not necessarily useful for diagnosis, since among other issues, it presents variations according to age [ 114 ].
Another example of the influence of age on brain electrical activity associated with ADHD is a study comparing children with and without ADHD, as well as adults with and without ADHD. Interestingly, children with ADHD presented higher delta and theta activity than control children, while in adults no difference was found between ADHD group and controls in the frequency bands analyzed [ 115 ]. Among the few differences in qEEG activity found in adults with ADHD is a higher gamma activity (39.25–48 Hz), suggesting a functional alteration in dorsal attention network [ 116 ].
ADHD patients often present comorbidities [ 117 ], which might influence qEEG in a different way to the findings in ADHD only patients. For example, children with ADHD and problematic Internet use present differences in qEEG when compared to ADHD only patients. However, no differences were found between ADHD only patients and ADHD patients with depression [ 118 ]. Another study found that adolescents with ADHD and Internet gaming disorder presented lower relative delta power and greater relative beta power than adolescents with ADHD only [ 119 ].
It is noteworthy that although a number of studies have been published regarding neurophysiological correlates of ADHD through qEEG, there are still some differences in the results reported by different authors. Beyond possible methodological differences, there are a number of factors reported to influence qEEG activity in ADHD patients, which might be responsible—at least in part—for the differences reported so far, and which might be of importance when using qEEG information to choose or design a therapeutic approach. These factors include comorbidities [ 4 , 120 ] and the ages of the patients [ 114 , 116 , 121 ]. Other factors reported to affect qEEG activity in other populations and conditions are ethnicity [ 122 , 123 , 124 , 125 , 126 ], sociocultural environment during development [ 127 , 128 ], and the degree of advancement of a psychiatric condition, as reported for alcohol dependence [ 129 , 130 , 131 ].
6. Therapeutic Approaches
6.1. pharmacological treatment.
Both stimulant and non-stimulant pharmacological treatments have proven to be effective in diminishing ADHD symptoms in children and adolescents [ 132 , 133 ], although stimulant medication seems to have greater effectiveness [ 133 , 134 ]. Herein, we will address one frequently used stimulant (methylphenidate) and one frequently used non-stimulant (atomoxetine)
6.1.1. Methylphenidate
Methylphenidate is one of the most used drugs for ADHD treatment. It has been present in the market for 50 years and it reduces excessive hyperactivity, impulsivity, and inattention in children and adolescents with ADHD. In the United States, it is prescribed to 8% of children and adolescents under 15 years of age and to around 3% to 5% of the same population in Europe [ 135 ].
Methylphenidate blocks DAT and NET, reducing reuptake and producing an increase in available dopamine and norepinephrine in the synaptic cleft [ 135 , 136 , 137 ], leading to increased dopamine and norepinephrine transmission in the prefrontal cortex [ 132 ]. A meta-analysis on the effects of methylphenidate treatment on ADHD in adults found it effective in improving neurocognitive performance, accomplishing better results than placebo groups in terms of working memory, reaction time variability, vigilance, driving, and response inhibition [ 136 ].
6.1.2. Atomoxetine
Atomoxetine has been reported to be effective for ADHD treatment [ 138 ], being more effective in adults than in children [ 134 ].
Atomoxetine blocks norepinephrine reuptake, producing increased presence of norepinephrine and dopamine in prefrontal cortex [ 132 ]. Since atomoxetine does not produce an increase of dopamine or norepinephrine in the nucleus accumbens, it lacks abuse potential [ 132 , 139 ]. This drug is associated with improvements in quality of life in children adolescents and adults, although this parameter is not further increased with long-term use [ 139 ].
6.1.3. Adverse Effects
Both stimulant and non-stimulant pharmacological treatments for ADHD produce adverse effects in a percentage of treated patients. The main adverse effects found for these drugs (% of patients treated with stimulants/% of patients treated with non-stimulants) are decreased appetite (28.6%/14.2%), nausea (7.9%/10.3%), headache (14.5%/20.8%), insomnia (12.3%/8.6%), nasopharyngitis (6.0%/7.1%), dizziness (5.1%/10.0%), abdominal pain (7.8%/11.5%), irritability (9.3%/6.9%), and somnolence (4.4%/34.1%) [ 133 ].
A systematic review on the adverse effects of methylphenidate in children and adolescents revealed that about 1 in 100 patients present serious adverse events after methylphenidate treatment (including death, cardiac problems and psychiatric disorders), while more than half of the patients treated with methylphenidate suffer one or more adverse events. The authors concluded that it is important to identify subgroups of patients who might be harmed by methylphenidate treatment and highlight the importance of remaining alert to possible adverse events in patients with this treatment [ 135 ]. There might also be uncommon adverse effects. For example, there is a report of 3 cases of systemic sclerosis associated with methylphenidate treatment [ 140 ]. The authors of the last study suggested that patients with signs of autoimmune or vasospastic conditions should be briefed about this possible side effect before commencing methylphenidate treatment.
A systematic review on possible adverse effects of atomoxetine, including decreased growth rate, cardiovascular and hepatic effects, aggression, psychosis, seizures, and suicidal ideation, determined that evidence indicates it is safe to use in ADHD patients [ 141 ]. Furthermore, the presence of comorbidities does not interfere with treatment efficacy, nor does treatment exacerbate comorbid symptoms [ 142 , 143 ]. However, it is important to be alert to other possible adverse effects. A case report and review indicated that the appearance of tics is a common side effect of atomoxetine treatment [ 144 ].
Methylphenidate and atomoxetine are known to increase heart rate and blood pressure, raising concern regarding possible cardiovascular effects of these drugs in ADHD patients. A review on the cardiovascular effects of these drugs in healthy subjects found the drug to be safe to use. Most of these studies were performed in children and adolescents, although there have also been some studies performed on adults, with no serious risk being reported in these subjects either. However, patient blood pressure and heart rate should be monitored on a regular basis. Moreover, careful follow-up should be performed for patients presenting certain cardiovascular conditions [ 145 ].
Weight loss has also been reported after atomoxetine treatment, occurring during the first two years of treatment. However, evidence suggests this decrease begins to be compensated between 2 and 5 years after the beginning of treatment [ 141 ]. Similarly, methylphenidate has been associated with adverse effects such as anorexia, weight loss, and insomnia [ 146 ].
A comparative study on short-term effects of methylphenidate and atomoxetine on ADHD reported significantly higher weight loss in children treated with atomoxetine [ 147 ]. However, a more recent study reported that children present significantly more weight loss after methylphenidate than after atomoxetine treatment [ 148 ].
A meta-analysis on gastrointestinal adverse effects of methylphenidate reported increased risk of decreased appetite, weight loss, and abdominal pain in children and adolescents under this pharmacological treatment [ 149 ].
A comparison between the presence of adverse effects after methylphenidate and atomoxetine treatments in ADHD children indicated methylphenidate as a safer option, since children under atomoxetine treatment presented higher incidence rates of anorexia, nausea, somnolence, dizziness, and vomiting than children under methylphenidate treatment [ 147 ]. A more recent study reported similar results, since children treated with atomoxetine presented higher incidence rates of mild adverse effects, such as decreased appetite, weight loss, dyspepsia, abdominal pain, stomach ache, irritability, mood disorders, and dizziness. As for severe adverse effects, patients under atomoxetine treatment presented higher incidence rates of gastrointestinal, neuropsychiatric, and cardiovascular effects [ 150 ].
6.1.4. Long-Term Adverse Effects
Long-term adverse effects of methylphenidate are the subject of intense study, given that it is the first-line stimulant drug used for ADHD treatment in children, adolescents, and adults [ 11 , 151 ]. A review on the subject addressed different adverse effects studied in patients after long-term (over one year) administration of methylphenidate, including low mood or depression, anxiety, irritability or emotional reactivity, suicidal behavior or ideation, bipolar disorder, psychotic symptoms, substance use disorders, tics, seizures or EEG abnormalities, and sleep disorders. The authors concluded that existing information indicates that methylphenidate is safe to use, although caution should be taken when prescribing this drug to specific groups, such as preschool children, patients prone to psychosis or tics, and high-risk adolescents [ 152 ]. However, the need for more studies on the long-term effects of treatment with this drug is highlighted, since studies in humans are rather scarce and with a high degree of heterogeneity in terms of methodological approach [ 151 , 152 ].
6.1.5. Long-Term Therapeutic Effect
Given that ADHD is a chronic disorder and that many of the children presenting ADHD will still present symptoms in adulthood, it is particularly important to determine the long-term effectiveness of pharmacological treatments. However, very few studies address this issue, and no conclusion can yet be drawn regarding the long-term effects (years) of pharmacological treatment of ADHD on symptom reduction and quality of life. Thus, the long-term efficacy of drug treatment for ADHD remains under debate [ 153 , 154 , 155 , 156 ]
Current pharmacological treatments for ADHD have proven to be safe and effective. The efficacy of these treatments on ADHD symptoms is clear, and thus pharmacological therapy is often used to treat ADHD patients [ 136 , 138 , 141 , 152 ]. However, there are also some drawbacks to this therapeutic approach, including the time required to reach the effective dose for each patient [ 3 , 157 ]; the lack of response in some patients [ 121 , 158 , 159 , 160 ]; the unresolved issue of long-term effectiveness (of great importance given that in many cases the treatment must go on for years) [ 153 , 154 , 155 , 156 ]; the presence of adverse effects, which although not life threatening in most cases, are nevertheless upsetting [ 133 , 135 , 144 ]; and the existence of specific groups of patients with whom a greater caution must be taken [ 140 , 145 , 152 ]. Altogether, these drawbacks have led to the search of new therapeutic approaches. One of the strategies studied so far is the possibility of using other drugs to treat ADHD, including drugs interacting with serotoninergic (metadoxine, paroxetine, duloxetine, buspirone), glutamatergic (memantine), cholinergic (AZD3480, AZD1446, lobeline, galantamine, mecamylamine), histaminergic (mk-0249), and catecholaminergic neurotransmission systems (modafinil, droxidopa, desipramine, bupropion, nomifensine, reboxetine, venlafaxine, duloxetine, guanfacine, aripiprazol, dasotraline, selegiline), as well as lithium [ 161 ].
6.2. Non-Pharmacological Therapies
Pharmacological therapy is effective although presents some inconveniences, including the existence of adverse effects in some patients and lack of effect in others. Therefore, there are also different non-pharmacological approaches for ADHD treatment.
6.2.1. Behavioral Parent Training
The goal of parent training is to equip parents with techniques that will be useful in managing ADHD-related behavior presented by their children. A systematic review published on 2011 found no reliable effect of ADHD children’s behavior, although it may lead to increased confidence and decreased stress in parents [ 162 ]. Later studies found an effect of behavioral parent training on ADHD symptoms, which is not increased by previous working memory training, although this combination did produce positive effects on working memory storage and processing [ 163 ]. It is noteworthy that cognitive functioning of both parents and children influences the effectiveness of this therapeutic approach on ADHD symptoms. Better working memory in children and higher parental response caution presented an association with improvements in inattention. As for conduct problems, better parental self-regulation was associated with a better result in this area. However, none of the measured cognitive functions in children or parents were associated with improvements in hyperactivity [ 164 ]. Moreover, behavioral parent training improves coexistence at home, since a reduction in the frequency and severity of problematic situations is produced, along with a reduction of stress in parents [ 165 ].
6.2.2. Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) has also been used to treat ADHD. A review performed on the subject found CBT to be effective in reducing ADHD symptoms in adults, however only when improvement was evaluated by the patient and not when evaluated by the clinician [ 166 ], although a more recent meta-analysis on the subject reported a good effect of CBT on ADHD adults [ 167 ]. A Cochrane systematic review concluded that CBT has a positive effect on ADHD symptoms, either alone or in conjunction with other therapies, although considered the evidence to be low-quality in accordance with the Grading of Recommendations Assessment, Development and Evaluation (GRADE) working group approach. [ 168 ]. A meta-analysis found that CBT is one of the most effective non-pharmacological options to treat ADHD, ranking just after physical exercise [ 169 ]. A later systematic review confirmed the effects of CBT on ADHD symptoms [ 170 ]. A recent study reported CBT to be effective in reducing ADHD symptoms in patients, either with or without conjunct medication [ 171 ].
6.2.3. Attention Training Techniques
Attention training techniques are often used to improve life quality and increase well-being. Given the effect of these techniques on brain activity, as well as on attention and self-regulation, their use to reduce ADHD symptoms and improve life quality in these patients is currently under study [ 172 ].
Mindfulness can be defined as paying attention to the present, an activity that implies sustained attention. A systematic review on the effects of mindfulness-based interventions on ADHD found that such approaches were popular among adults with ADHD, finding improvements in attention, although the effects of such approaches in children and adolescents are still unclear [ 173 ]. A recent meta-review reported a large effect size of mindfulness on ADHD [ 174 ]. A review on the effects of mindfulness-based cognitive therapy on ADHD adults reported good effects of this therapeutic approach, especially when used in conjunction with pharmacological therapy [ 175 ], while a systematic review analyzing the effects of meditation-based techniques (either on parents and children or on children only) on ADHD children could not draw a clear conclusion regarding beneficial effects [ 176 ].
Adult ADHD patients that underwent an 8-week mindfulness awareness practice period presented decreased ADHD, depression, and anxiety symptoms [ 177 ]. Similarly, a study performed with children revealed that an 8-week period of mindfulness-oriented meditation produced improvements in the performance of neuropsychological tests, as well as in ADHD symptoms. Although encouraging, the authors stated that the results are still preliminary, given the small number of children participating in the study [ 178 ]. There are also results indicating that this technique produces an improvement in ADHD symptoms in ADHD children with oppositional defiant disorder [ 179 ].
6.2.4. Neurofeedback
Neurofeedback (NFB) is a therapy in which patients learn to modify EEG patterns through operant conditioning. There are articles reporting the induction of plastic changes after NFB training [ 180 , 181 , 182 , 183 ], supporting a theory explaining the effects of NFB on different brain disorders through the induction of synaptic plasticity, leading to an homeostatic set point. Additionally, besides some unusual cases of headache, no collateral effects have been reported with this technique. One of the most interesting aspects of NFB is the induction of plastic changes from within the brain under normal physiological conditions, without the need for an external stimuli such as pharmacological treatments or transcranial stimulation to alter brain activity, thus the probability of adverse effects is minimal [ 181 ].
Specific NFB protocols have been developed over the decades. These protocols were designed based on articles reporting specific qEEG variations in neurological patients or qEEG patterns associated with cognitive function. Some of these standardized protocols have been studied in terms of their ability to treat ADHD [ 184 ].
Several articles have addressed the use of NFB in ADHD patients. The results have been mixed and numerous meta-analyses have been published on the subject. The conclusions of these meta-analyses have also been mixed. There are meta-analyses reporting good effects of NFB on ADHD [ 185 , 186 , 187 ], not finding reliable effects [ 188 ], not reaching a conclusion on the subject of efficacy [ 189 ], finding a minor effect of this therapeutic approach significantly below what is observed with pharmacological treatment [ 190 ], or finding a minor effect only in the presence of pharmacological treatment [ 191 ].
An overview of recent publications gave the same impression. Some reports found effects of NFB theta/beta or theta/alpha protocols on ADHD, measurable at follow-up 8 weeks or 12 months after treatment completion [ 192 , 193 ]. Other reports found no effect [ 194 , 195 , 196 ]. Moreover, there are reports revealing a minor effect of NFB, below the effect levels of other therapeutic approaches [ 197 , 198 , 199 ].
NFB is a therapeutic approach widely studied for ADHD treatment. The results so far have been mixed. However, given the absence of side effects and its ability to induce synaptic plasticity [ 181 ], it is an option worth keeping in mind.
6.2.5. Other Non-Pharmacological Approaches
The use of non-pharmacological supplementations, such as polyunsaturated fatty acids, peptides, amino acids, plat extracts, probiotics, micronutrients, and herbal supplementation, is currently being studied in order to determine their usefulness in treating ADHD. However, further research is still needed in this area [ 200 ].
A study performed in ADHD children under methylphenidate treatment for whom zinc supplementation was added reported no significant effect of zinc supplementation on the total score for a parent’s questionnaire for ADHD or in the hyperactivity and impulsivity subscales. However, zinc-supplemented children present improvements in inattention scores [ 201 ].
A meta-analysis on non-pharmacological interventions for ADHD patients found that physical exercise produced a good effect on ADHD cognitive symptoms, especially aerobic exercise targeting executive functions [ 169 ].
7. Treatment Personalization
In the first sections of this review, we addressed some of the factors associated with ADHD incidence, ranging from a variety of environmental factors to the presence of different genetic polymorphisms. However, these different etiologies are not always present, since patients might present one or another (see Section 2 and Section 3 ). Similarly, while there are some changes in brain activity associated with ADHD, they are not always the same (see Section 4 ). Accordingly, there is also variation in the response of patients to both pharmacological and non-pharmacological treatments (see Section 5 ).
Since the etiology of ADHD could be very different from patient to patient, the precise nature of the physiological changes underlying the clinical manifestations of ADHD in each case could be slightly different, affecting the effectiveness of the chosen treatment and possibly explaining the variation in the effect of the same treatment on different patients. This can be observed in the variations in qEEG activity observed in different studies [ 112 , 113 , 114 , 116 , 121 ]. However, the design of personalized treatments based on specific characteristics of each patient could lead to better clinical results. In this regard, strategies to adjust therapeutic approaches based on patients’ characteristics have been used for both pharmacological and non-pharmacological therapies.
Selecting the appropriate pharmacological treatment and the dose to be used takes some time, given the large inter-individual variability regarding treatment efficacy, leading to a delay in reaching a therapeutic effect, and in some cases producing an early termination of treatment due to frustration, either by the provider or the family [ 157 ]. Moreover, there is some variability regarding patient response to methylphenidate, including patients that do not achieve adequate symptom control or experience adverse effects with commonly used doses. Therefore, dose optimization has been proposed as a means to achieve an adequate effect for most of the patients, enhancing both the efficacy and safety of methylphenidate treatment [ 3 ]. This has led to the search for strategies to find adequate treatments for each patient, such as pharmacogenomics, in which a patient’s genotype for a particular gene is used to predict the effects of medication in that patient. However, in spite of the progress that has already been made, no pharmacogenomic test so far has been found to be helpful in treatment selection [ 157 ].
Treatment resistance has been reported for both atomoxetine [ 158 ] and methylphenidate [ 121 , 159 , 160 ]. For this reason, qEEG can be used as a source of information to determine at an earlier point whether methylphenidate [ 121 , 160 , 202 ] or atomoxetine [ 107 , 202 ] is effective or if an alternative treatment is needed for a patient.
Most of the reports on the use of NFB for ADHD use a standardized protocol, either equal for all participants or adapted to each patients after qEEG analysis. However, there is another more personalized approach known as qEEG-informed (or qEEG-guided) NFB. In this variant of NFB, rather than selecting a particular protocol (for example, theta/beta ratio) and applying it to all participants, subjects receive a NFB protocol selected for them after qEEG analysis. This type of NFB has been successfully used in schizophrenia [ 203 ], obsessive compulsive disorder [ 204 ], migraine [ 205 ], dementia [ 206 ], and with learning-disabled children [ 207 , 208 ].
There are so far only two studies applying qEEG-informed NFB in ADHD patients, so it is not yet possible to perform a meta-analysis on the effects of this type of NFB on ADHD. However, a positive effect of NFB has been reported in both published studies [ 209 , 210 ].
8. Discussion
ADHD is an NDD with a complex etiology. While it is clear that its main cause is alterations in neurodevelopmental processes such as synaptogenesis, myelination, and neurogenesis [ 5 ], the causes of these neurodevelopmental alterations are diverse. In some cases they might be associated with environmental factors such as premature birth [ 6 ], perinatal problems [ 9 ], nutrition during pregnancy [ 10 ], or exposure to heavy metals [ 17 , 18 , 19 , 26 , 27 , 29 ]. Additionally, there is strong evidence of genetic influence on ADHD [ 43 , 44 ], and an interaction between environmental and genetic factors cannot be discarded.
The purpose of this review is not to fully describe all factors associated with ADHD appearance, but rather to address some of the main etiologies described so far, in order to clarify the high diversity of factors associated with this NDD. When analyzing the different sections of this review, one thing becomes evident—that ADHD patients are diverse regarding the etiology of their condition and their responses to treatment. This heterogeneity outlines the high variability in patients’ particular conditions regarding ADHD symptom manifestation and treatment, since it is probable that the underlying neurophysiological alterations for each patient are at least slightly different. Thus, standardized treatment (either pharmacological or non-pharmacological) may not be equally efficient in all cases.
Moreover, there could be other factors that are usually disregarded in relation with ADHD incidence, but which might play an important role in this condition. Recently, the gut microbiome has been the subject of intense research as an ADHD-associated factor, and even though further research is needed in order to determine its precise influence on ADHD, there are already reports indicating a possible link between them [ 211 , 212 , 213 , 214 ].
In the end, all of these factors produce changes in brain structure and function [ 1 , 7 , 112 , 113 , 114 , 115 ], leading to the symptomatology observed in ADHD patients. Therapeutic approaches to treat this condition have the objective of compensating such alterations in order to reduce symptoms and improve quality of life. However, as we have observed in this review, not all patients present the same neurophysiological changes. Studies performed on qEEG activity have yielded different results regarding brain electrical activity in ADHD patients [ 4 , 112 , 114 , 120 ]. Additionally, both brain imaging and qEEG techniques have revealed that changes are not consistent throughout the lifespan, being different in children and adults [ 114 , 115 , 116 , 121 ]. Therefore, there is a need for treatment personalization for each ADHD patient in order to achieve greater effect with minimal adverse effects.
Pharmacological treatments, both stimulants and non-stimulants have proven to be effective and safe for ADHD patients [ 132 , 133 ], and thus are widely prescribed to treat this condition. However, the pharmacological approach to ADHD treatment has some drawbacks, mostly regarding difficulties in reaching effectiveness in all patients [ 3 , 121 , 157 , 158 , 159 , 160 ] and the presence of adverse effects [ 133 , 135 , 144 ].
The search for other therapeutic options has led to the assessment of the effects of other drugs on ADHD [ 161 ], as well as the design of non-pharmacological treatments, such as behavioral parent training, CBT, attention-improving techniques, and NFB.
The effects of behavioral parent training on ADHD symptoms in children are not consistent, with some articles finding effects [ 163 ] and others not finding any [ 162 ]. However, behavioral parent training does reduce stress in parents and promotes a better coexistence at home, which is favorable for children [ 162 , 165 ]. In the case of CBT, there is more evidence indicating a good effect in reducing ADHD symptoms [ 167 , 168 , 169 , 170 , 171 ]
Attention training techniques are still under intense study. There is some evidence regarding the effect of this technique on ADHD in adults [ 173 , 175 ], while in children and adolescents the results are not clear so far [ 173 , 176 ].
A number of studies on the effect of NFB on ADHD symptoms have yielded different results, either finding a positive effect [ 185 , 186 , 187 , 192 , 193 ], a mild effect [ 190 , 197 , 198 , 199 ], or no effect at all [ 188 , 194 , 195 , 196 ]. However, NFB has a number of advantages that encourage the search for an adequate protocol to treat ADHD patients. It is targeted directly to change brain activity associated with the condition under treatment, it has virtually no side effects, and the therapeutic effect is due to the induction of plastic changes in the central nervous system, thus it might establish a long-term changes [ 180 , 181 , 182 , 183 ].
9. Conclusions
In the present review, we have gone through some of the factors associated with ADHD, and it is clear that a great heterogeneity exists in the etiology of this condition. Therapeutic approaches, although functional in many cases, also show heterogeneity in their effects in certain groups of patients. The diverse range of effects of the therapeutic approaches used should not be a surprise, given the diversity of etiologies found in ADHD. Even though clinical manifestations of this condition might be similar (diagnosis is based on the presence certain symptoms), the same clinical manifestations could occur with different underlying physiological changes, considering the variations in qEEG activity in different groups of patients [ 112 , 113 , 114 , 116 , 121 ]. Thus, these neurophysiological changes presented by patients may not necessarily respond in equal form to a given therapeutic approach. Given the inter-personal variance in the etiology of ADHD, it is advisable to personalize the therapeutic approach. Regarding pharmacological therapies, dosage optimization [ 3 ], pharmacogenomics [ 157 ], and the use of qEEG to select the adequate drug for a given patient have been proposed [ 107 , 121 , 160 , 202 ].
Regarding non-pharmacological options, the use of qEEG-informed NFB has been proposed for personalized treatment in ADHD patients. The studies carried out to date have shown positive results [ 209 , 210 ], although the number of studies is still too small to draw a conclusion. However, given the advantages of NFB [ 181 ] and the positive effects of this approach reported for other conditions [ 203 , 204 , 205 , 206 , 207 , 208 ], it is worth performing further studies on the effectiveness of this type of NFB on ADHD.

Author Contributions
Conceptualization, L.N.-J. and W.V.H.-M. writing—reviewing and editing, L.N.-J., W.V.H.-M., and A.H.-S. All authors have read and agreed to the published version of the manuscript.
This research received no external funding
Conflicts of Interest
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- 1. Delgado-Mejia I.D., Palencia-Avendano M.L., Mogollon-Rincon C., Etchepareborda M.C. Theta/beta ratio (NEBA) in the diagnosis of attention deficit hyperactivity disorder. Rev. Neurol. 2014;58(Suppl. S1):S57–S63. [ PubMed ] [ Google Scholar ]
- 2. Rodrak S., Wongsawat Y. EEG brain mapping and brain connectivity index for subtypes classification of attention deficit hyperactivity disorder children during the eye-opened period; Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC); Osaka, Japan. 3–7 July 2013; pp. 7400–7403. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Huss M., Duhan P., Gandhi P., Chen C.W., Spannhuth C., Kumar V. Methylphenidate dose optimization for ADHD treatment: Review of safety, efficacy, and clinical necessity. Neuropsychiatr. Dis. Treat. 2017;13:1741–1751. doi: 10.2147/NDT.S130444. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Ortíz León S., Jaimes Medrano A.L. Trastorno por déficit de atención en la edad adulta y en universitarios. Revista de la Facultad de Medicina de la UNAM. 2016;59:6–14. [ Google Scholar ]
- 5. Homberg J.R., Kyzar E.J., Nguyen M., Norton W.H., Pittman J., Poudel M.K., Gaikwad S., Nakamura S., Koshiba M., Yamanouchi H., et al. Understanding autism and other neurodevelopmental disorders through experimental translational neurobehavioral models. Neurosci. Biobehav. Rev. 2016;65:292–312. doi: 10.1016/j.neubiorev.2016.03.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Aylward G.P. Neurodevelopmental outcomes of infants born prematurely. J. Dev. Behav. Pediatr. 2005;26:427–440. doi: 10.1097/00004703-200512000-00008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Ambrosino S., de Zeeuw P., Wierenga L.M., van Dijk S., Durston S. What can Cortical Development in Attention-Deficit/Hyperactivity Disorder Teach us About the Early Developmental Mechanisms Involved? Cereb. Cortex. 2017;27:4624–4634. doi: 10.1093/cercor/bhx182. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Allred E.N., Dammann O., Fichorova R.N., Hooper S.R., Hunter S.J., Joseph R.M., Kuban K., Leviton A., O’Shea T.M., Scott M.N., et al. Systemic Inflammation during the First Postnatal Month and the Risk of Attention Deficit Hyperactivity Disorder Characteristics among 10 year-old Children Born Extremely Preterm. J. Neuroimmune Pharmacol. 2017;12:531–543. doi: 10.1007/s11481-017-9742-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Giannopoulou I., Pagida M.A., Briana D.D., Panayotacopoulou M.T. Perinatal hypoxia as a risk factor for psychopathology later in life: The role of dopamine and neurotrophins. Hormones. 2018;17:25–32. doi: 10.1007/s42000-018-0007-7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Gharami K., Das M., Das S. Essential role of docosahexaenoic acid towards development of a smarter brain. Neurochem. Int. 2015;89:51–62. doi: 10.1016/j.neuint.2015.08.014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Bonvicini C., Faraone S.V., Scassellati C. Attention-deficit hyperactivity disorder in adults: A systematic review and meta-analysis of genetic, pharmacogenetic and biochemical studies. Mol. Psychiatry. 2016;21:872–884. doi: 10.1038/mp.2016.74. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Udagawa J., Hino K. Impact of Maternal Stress in Pregnancy on Brain Function of the Offspring. Nihon Eiseigaku Zasshi. 2016;71:188–194. doi: 10.1265/jjh.71.188. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Choi C.S., Kim P., Park J.H., Gonzales E.L., Kim K.C., Cho K.S., Ko M.J., Yang S.M., Seung H., Han S.H., et al. High sucrose consumption during pregnancy induced ADHD-like behavioral phenotypes in mice offspring. J. Nutr. Biochem. 2015;26:1520–1526. doi: 10.1016/j.jnutbio.2015.07.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Choi I., Kim P., Joo S.H., Kim M.K., Park J.H., Kim H.J., Ryu J.H., Cheong J.H., Shin C.Y. Effects of Preconceptional Ethanol Consumption on ADHD-Like Symptoms in Sprague-Dawley Rat Offsprings. Biomol. Ther. 2012;20:226–233. doi: 10.4062/biomolther.2012.20.2.226. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Kim P., Choi C.S., Park J.H., Joo S.H., Kim S.Y., Ko H.M., Kim K.C., Jeon S.J., Park S.H., Han S.H., et al. Chronic exposure to ethanol of male mice before mating produces attention deficit hyperactivity disorder-like phenotype along with epigenetic dysregulation of dopamine transporter expression in mouse offspring. J. Neurosci. Res. 2014;92:658–670. doi: 10.1002/jnr.23275. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Richardson J.R., Taylor M.M., Shalat S.L., Guillot T.S., 3rd, Caudle W.M., Hossain M.M., Mathews T.A., Jones S.R., Cory-Slechta D.A., Miller G.W. Developmental pesticide exposure reproduces features of attention deficit hyperactivity disorder. FASEB J. 2015;29:1960–1972. doi: 10.1096/fj.14-260901. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Barry M.J., Almotawah F., Pani S.C., Ingle N.A. A Comparison of Salivary Mercury Levels in Children with Attention Deficit/Hyperactivity Disorder When Compared to Age-matched Controls: A Case-control Observational Study. J. Contemp. Dent. Pract. 2020;21:129–132. [ PubMed ] [ Google Scholar ]
- 18. Bhang S.Y., Cho S.C., Kim J.W., Hong Y.C., Shin M.S., Yoo H.J., Cho I.H., Kim Y., Kim B.N. Relationship between blood manganese levels and children’s attention, cognition, behavior, and academic performance--a nationwide cross-sectional study. Environ. Res. 2013;126:9–16. doi: 10.1016/j.envres.2013.05.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Schullehner J., Thygesen M., Kristiansen S.M., Hansen B., Pedersen C.B., Dalsgaard S. Exposure to Manganese in Drinking Water during Childhood and Association with Attention-Deficit Hyperactivity Disorder: A Nationwide Cohort Study. Environ. Health Perspect. 2020;128:97004. doi: 10.1289/EHP6391. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Chan T.J., Gutierrez C., Ogunseitan O.A. Metallic Burden of Deciduous Teeth and Childhood Behavioral Deficits. Int. J. Environ. Res. Public Health. 2015;12:6771–6787. doi: 10.3390/ijerph120606771. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Liu W., Huo X., Liu D., Zeng X., Zhang Y., Xu X. S100beta in heavy metal-related child attention-deficit hyperactivity disorder in an informal e-waste recycling area. Neurotoxicology. 2014;45:185–191. doi: 10.1016/j.neuro.2014.10.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Nigg J.T., Knottnerus G.M., Martel M.M., Nikolas M., Cavanagh K., Karmaus W., Rappley M.D. Low blood lead levels associated with clinically diagnosed attention-deficit/hyperactivity disorder and mediated by weak cognitive control. Biol. Psychiatry. 2008;63:325–331. doi: 10.1016/j.biopsych.2007.07.013. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Nigg J.T., Nikolas M., Mark Knottnerus G., Cavanagh K., Friderici K. Confirmation and extension of association of blood lead with attention-deficit/hyperactivity disorder (ADHD) and ADHD symptom domains at population-typical exposure levels. J. Child Psychol. Psychiatry. 2010;51:58–65. doi: 10.1111/j.1469-7610.2009.02135.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Nigg J.T., Elmore A.L., Natarajan N., Friderici K.H., Nikolas M.A. Variation in an Iron Metabolism Gene Moderates the Association Between Blood Lead Levels and Attention-Deficit/Hyperactivity Disorder in Children. Psychol. Sci. 2016;27:257–269. doi: 10.1177/0956797615618365. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Wang T., Zhang J., Xu Y. Epigenetic Basis of Lead-Induced Neurological Disorders. Int. J. Environ. Res. Public Health. 2020;17:4878. doi: 10.3390/ijerph17134878. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Munoz M.P., Rubilar P., Valdes M., Munoz-Quezada M.T., Gomez A., Saavedra M., Iglesias V. Attention deficit hyperactivity disorder and its association with heavy metals in children from northern Chile. Int. J. Hyg. Environ. Health. 2020;226:113483. doi: 10.1016/j.ijheh.2020.113483. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Sanders A.P., Claus Henn B., Wright R.O. Perinatal and Childhood Exposure to Cadmium, Manganese, and Metal Mixtures and Effects on Cognition and Behavior: A Review of Recent Literature. Curr. Environ. Health Rep. 2015;2:284–294. doi: 10.1007/s40572-015-0058-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Kim W., Jang Y., Lim Y.H., Kim B.N., Shin C.H., Lee Y.A., Kim J.I., Hong Y.C. The Effect of Prenatal Cadmium Exposure on Attention-deficit/Hyperactivity Disorder in 6-Year-old Children in Korea. J. Prev. Med. Public Health. 2020;53:29–36. doi: 10.3961/jpmph.19.175. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Li Y., Cha C., Lv X., Liu J., He J., Pang Q., Meng L., Kuang H., Fan R. Association between 10 urinary heavy metal exposure and attention deficit hyperactivity disorder for children. Environ. Sci. Pollut. Res. Int. 2020;27:31233–31242. doi: 10.1007/s11356-020-09421-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Skalny A.V., Mazaletskaya A.L., Ajsuvakova O.P., Bjorklund G., Skalnaya M.G., Chao J.C., Chernova L.N., Shakieva R.A., Kopylov P.Y., Skalny A.A., et al. Serum zinc, copper, zinc-to-copper ratio, and other essential elements and minerals in children with attention deficit/hyperactivity disorder (ADHD) J. Trace Elem. Med. Biol. 2020;58:126445. doi: 10.1016/j.jtemb.2019.126445. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Luo J., Mo Y., Liu M. Blood and hair zinc levels in children with attention deficit hyperactivity disorder: A meta-analysis. Asian J. Psychiatr. 2020;47:101805. doi: 10.1016/j.ajp.2019.09.023. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Bijlenga D., Vollebregt M.A., Kooij J.J.S., Arns M. The role of the circadian system in the etiology and pathophysiology of ADHD: Time to redefine ADHD? Atten. Defic. Hyperact. Disord. 2019;11:5–19. doi: 10.1007/s12402-018-0271-z. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Snitselaar M.A., Smits M.G., van der Heijden K.B., Spijker J. Sleep and Circadian Rhythmicity in Adult ADHD and the Effect of Stimulants. J. Atten. Disord. 2017;21:14–26. doi: 10.1177/1087054713479663. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Chamorro M., Lara J.P., Insa I., Espadas M., Alda-Diez J.A. Evaluation and treatment of sleep problems in children diagnosed with attention deficit hyperactivity disorder: An update of the evidence. Rev. Neurol. 2017;64:413–421. [ PubMed ] [ Google Scholar ]
- 35. Wajszilber D., Santiseban J.A., Gruber R. Sleep disorders in patients with ADHD: Impact and management challenges. Nat. Sci. Sleep. 2018;10:453–480. doi: 10.2147/NSS.S163074. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Hvolby A. Associations of sleep disturbance with ADHD: Implications for treatment. Atten. Defic. Hyperact. Disord. 2015;7:1–18. doi: 10.1007/s12402-014-0151-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Weibel S., Menard O., Ionita A., Boumendjel M., Cabelguen C., Kraemer C., Micoulaud-Franchi J.A., Bioulac S., Perroud N., Sauvaget A., et al. Practical considerations for the evaluation and management of Attention Deficit Hyperactivity Disorder (ADHD) in adults. Encephale. 2020;46:30–40. doi: 10.1016/j.encep.2019.06.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Lugo J., Fadeuilhe C., Gisbert L., Setien I., Delgado M., Corrales M., Richarte V., Ramos-Quiroga J.A. Sleep in adults with autism spectrum disorder and attention deficit/hyperactivity disorder: A systematic review and meta-analysis. Eur. Neuropsychopharmacol. 2020;38:1–24. doi: 10.1016/j.euroneuro.2020.07.004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Singh K., Zimmerman A.W. Sleep in Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder. Semin. Pediatr. Neurol. 2015;22:113–125. doi: 10.1016/j.spen.2015.03.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Owens J.A. Sleep disorders and attention-deficit/hyperactivity disorder. Curr. Psychiatry Rep. 2008;10:439–444. doi: 10.1007/s11920-008-0070-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Tsai M.H., Huang Y.S. Attention-deficit/hyperactivity disorder and sleep disorders in children. Med. Clin. N. Am. 2010;94:615–632. doi: 10.1016/j.mcna.2010.03.008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 42. Perez A., Hunter K. Adenotonsillectomy as a treatment for sleep-disordered breathing in children with ADHD. JAAPA. 2020;33:34–39. doi: 10.1097/01.JAA.0000697248.35685.c6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 43. Faraone S.V., Perlis R.H., Doyle A.E., Smoller J.W., Goralnick J.J., Holmgren M.A., Sklar P. Molecular genetics of attention-deficit/hyperactivity disorder. Biol. Psychiatry. 2005;57:1313–1323. doi: 10.1016/j.biopsych.2004.11.024. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Demontis D., Walters R.K., Martin J., Mattheisen M., Als T.D., Agerbo E., Baldursson G., Belliveau R., Bybjerg-Grauholm J., Baekvad-Hansen M., et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat. Genet. 2019;51:63–75. doi: 10.1038/s41588-018-0269-7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 45. Martinez-Morga M., Quesada-Rico M.P., Bueno C., Martinez S. Neurobiological bases of autistic spectrum disorder and attention deficit hyperactivity disorder: Neural differentiation and synaptogenesis. Rev. Neurol. 2018;66:S97–S102. [ PubMed ] [ Google Scholar ]
- 46. Liu D.Y., Shen X.M., Yuan F.F., Guo O.Y., Zhong Y., Chen J.G., Zhu L.Q., Wu J. The Physiology of BDNF and Its Relationship with ADHD. Mol. Neurobiol. 2015;52:1467–1476. doi: 10.1007/s12035-014-8956-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Galvez-Contreras A.Y., Campos-Ordonez T., Gonzalez-Castaneda R.E., Gonzalez-Perez O. Alterations of Growth Factors in Autism and Attention-Deficit/Hyperactivity Disorder. Front. Psychiatry. 2017;8:126. doi: 10.3389/fpsyt.2017.00126. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Saadat F., Kosha M., Amiry A., Torabi G. Brain-derived neurotrophic factor as a biomarker in children with attention deficit-hyperactivity disorder. J. Krishna Inst. Med. Sci. Univ. 2015;4:10–17. [ Google Scholar ]
- 49. Corominas-Roso M., Ramos-Quiroga J.A., Ribases M., Sanchez-Mora C., Palomar G., Valero S., Bosch R., Casas M. Decreased serum levels of brain-derived neurotrophic factor in adults with attention-deficit hyperactivity disorder. Int. J. Neuropsychopharmacol. 2013;16:1267–1275. doi: 10.1017/S1461145712001629. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Amiri A., Torabi Parizi G., Kousha M., Saadat F., Modabbernia M.J., Najafi K., Atrkar Roushan Z. Changes in plasma Brain-derived neurotrophic factor (BDNF) levels induced by methylphenidate in children with Attention deficit-hyperactivity disorder (ADHD) Prog. Neuropsychopharmacol. Biol. Psychiatry. 2013;47:20–24. doi: 10.1016/j.pnpbp.2013.07.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Akay A.P., Resmi H., Guney S.A., Erkuran H.O., Ozyurt G., Sargin E., Topuzoglu A., Tufan A.E. Serum brain-derived neurotrophic factor levels in treatment-naive boys with attention-deficit/hyperactivity disorder treated with methylphenidate: An 8-week, observational pretest-posttest study. Eur. Child. Adolesc. Psychiatry. 2018;27:127–135. doi: 10.1007/s00787-017-1022-y. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Simsek S., Gencoglan S., Yuksel T., Kaplan I., Aktas H., Alaca R. Evaluation of the Relationship between Brain-Derived Neurotropic Factor Levels and the Stroop Interference Effect in Children with Attention-Deficit Hyperactivity Disorder. Noro Psikiyatr. Ars. 2016;53:348–352. doi: 10.5152/npa.2016.10234. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 53. Bilgic A., Toker A., Isik U., Kilinc I. Serum brain-derived neurotrophic factor, glial-derived neurotrophic factor, nerve growth factor, and neurotrophin-3 levels in children with attention-deficit/hyperactivity disorder. Eur. Child. Adolesc. Psychiatry. 2017;26:355–363. doi: 10.1007/s00787-016-0898-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. Sahin S., Yuce M., Alacam H., Karabekiroglu K., Say G.N., Salis O. Effect of methylphenidate treatment on appetite and levels of leptin, ghrelin, adiponectin, and brain-derived neurotrophic factor in children and adolescents with attention deficit and hyperactivity disorder. Int. J. Psychiatry Clin. Pract. 2014;18:280–287. doi: 10.3109/13651501.2014.940054. [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Zhang J., Luo W., Li Q., Xu R., Wang Q., Huang Q. Peripheral brain-derived neurotrophic factor in attention-deficit/hyperactivity disorder: A comprehensive systematic review and meta-analysis. J. Affect. Disord. 2018;227:298–304. doi: 10.1016/j.jad.2017.11.012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. Cubero-Millan I., Ruiz-Ramos M.J., Molina-Carballo A., Martinez-Serrano S., Fernandez-Lopez L., Machado-Casas I., Tortosa-Pinto P., Ruiz-Lopez A., Luna-Del-Castillo J.D., Uberos J., et al. BDNF concentrations and daily fluctuations differ among ADHD children and respond differently to methylphenidate with no relationship with depressive symptomatology. Psychopharmacology. 2017;234:267–279. doi: 10.1007/s00213-016-4460-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Ozturk O., Basay B.K., Buber A., Basay O., Alacam H., Bacanli A., Yilmaz S.G., Erdal M.E., Herken H., Ercan E.S. Brain-Derived Neurotrophic Factor Gene Val66Met Polymorphism Is a Risk Factor for Attention-Deficit Hyperactivity Disorder in a Turkish Sample. Psychiatry Investig. 2016;13:518–525. doi: 10.4306/pi.2016.13.5.518. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. Aureli A., Del Beato T., Sebastiani P., Marimpietri A., Melillo C.V., Sechi E., Di Loreto S. Attention-deficit hyperactivity disorder and intellectual disability: A study of association with brain-derived neurotrophic factor gene polymorphisms. Int. J. Immunopathol. Pharmacol. 2010;23:873–880. doi: 10.1177/039463201002300323. [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. Lanktree M., Squassina A., Krinsky M., Strauss J., Jain U., Macciardi F., Kennedy J.L., Muglia P. Association study of brain-derived neurotrophic factor (BDNF) and LIN-7 homolog (LIN-7) genes with adult attention-deficit/hyperactivity disorder. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2008;147B:945–951. doi: 10.1002/ajmg.b.30723. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Lee Y.H., Song G.G. BDNF 196 G/A and COMT Val158Met Polymorphisms and Susceptibility to ADHD: A Meta-Analysis. J. Atten. Disord. 2018;22:872–877. doi: 10.1177/1087054715570389. [ DOI ] [ PubMed ] [ Google Scholar ]
- 61. Xu X., Mill J., Zhou K., Brookes K., Chen C.K., Asherson P. Family-based association study between brain-derived neurotrophic factor gene polymorphisms and attention deficit hyperactivity disorder in UK and Taiwanese samples. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2007;144B:83–86. doi: 10.1002/ajmg.b.30406. [ DOI ] [ PubMed ] [ Google Scholar ]
- 62. Kwon H.J., Ha M., Jin H.J., Hyun J.K., Shim S.H., Paik K.C., Park W.S., Lim M.H. Association between BDNF gene polymorphisms and attention deficit hyperactivity disorder in Korean children. Genet. Test. Mol. Biomark. 2015;19:366–371. doi: 10.1089/gtmb.2015.0029. [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Luo L., Jiang X., Cao G., Xiong P., Yang R., Zhang J., Shen M. Association between BDNF gene polymorphisms and attention deficit hyperactivity disorder in school-aged children in Wuhan, China. J. Affect. Disord. 2020;264:304–309. doi: 10.1016/j.jad.2020.01.017. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Wang N., Wang Z., Yan F., Fu W. Correlation between single nucleotide polymorphisms of neurotrophic factors and executive function characteristics in children with attention deficit hyperactivity disorder. Wei Sheng Yan Jiu. 2019;48:577–582. [ PubMed ] [ Google Scholar ]
- 65. Cho S.C., Kim H.W., Kim B.N., Kim J.W., Shin M.S., Chung S., Cho D.Y., Jung S.W., Yoo H.J., Chung I.W., et al. Gender-specific association of the brain-derived neurotrophic factor gene with attention-deficit/hyperactivity disorder. Psychiatry Investig. 2010;7:285–290. doi: 10.4306/pi.2010.7.4.285. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 66. Hawi Z., Cummins T.D., Tong J., Arcos-Burgos M., Zhao Q., Matthews N., Newman D.P., Johnson B., Vance A., Heussler H.S., et al. Rare DNA variants in the brain-derived neurotrophic factor gene increase risk for attention-deficit hyperactivity disorder: A next-generation sequencing study. Mol. Psychiatry. 2017;22:580–584. doi: 10.1038/mp.2016.117. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Viikki M.L., Jarventausta K., Leinonen E., Huuhka M., Mononen N., Lehtimaki T., Kampman O. BDNF polymorphism rs11030101 is associated with the efficacy of electroconvulsive therapy in treatment-resistant depression. Psychiatr. Genet. 2013;23:134–136. doi: 10.1097/YPG.0b013e328360c894. [ DOI ] [ PubMed ] [ Google Scholar ]
- 68. Tsai A., Liou Y.J., Hong C.J., Wu C.L., Tsai S.J., Bai Y.M. Association study of brain-derived neurotrophic factor gene polymorphisms and body weight change in schizophrenic patients under long-term atypical antipsychotic treatment. Neuromol. Med. 2011;13:328–333. doi: 10.1007/s12017-011-8159-5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 69. Licinio J., Dong C., Wong M.L. Novel sequence variations in the brain-derived neurotrophic factor gene and association with major depression and antidepressant treatment response. Arch. Gen. Psychiatry. 2009;66:488–497. doi: 10.1001/archgenpsychiatry.2009.38. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 70. Pae C.U., Chiesa A., Porcelli S., Han C., Patkar A.A., Lee S.J., Park M.H., Serretti A., De Ronchi D. Influence of BDNF variants on diagnosis and response to treatment in patients with major depression, bipolar disorder and schizophrenia. Neuropsychobiology. 2012;65:1–11. doi: 10.1159/000327605. [ DOI ] [ PubMed ] [ Google Scholar ]
- 71. Ye C.Y., Xu Y.Q., Hu H., Yu S.Y., Wang D.X., Shi S.X., Wang L.W. An association study of brain-derived neurotrophic factor gene polymorphism in bipolar disorders. Zhonghua Yi Xue Za Zhi. 2009;89:1897–1901. [ PubMed ] [ Google Scholar ]
- 72. Xie B., Wang B., Suo P., Kou C., Wang J., Meng X., Cheng L., Ma X., Yu Y. Genetic association between BDNF gene polymorphisms and phobic disorders: A case-control study among mainland Han Chinese. J. Affect. Disord. 2011;132:239–242. doi: 10.1016/j.jad.2010.12.017. [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. Aldoghachi A.F., Tor Y.S., Redzun S.Z., Lokman K.A.B., Razaq N.A.A., Shahbudin A.F., Badamasi I.M., Cheah P.S., Stanslas J., Veerakumarasivam A., et al. Screening of brain-derived neurotrophic factor (BDNF) single nucleotide polymorphisms and plasma BDNF levels among Malaysian major depressive disorder patients. PLoS ONE. 2019;14:e0211241. doi: 10.1371/journal.pone.0211241. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 74. Liu X., Xu Y., Jiang S., Cui D., Qian Y., Jiang K. Family-based association study between brain-derived neurotrophic factor gene and major depressive disorder of Chinese descent. Psychiatry Res. 2009;169:169–172. doi: 10.1016/j.psychres.2008.06.014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 75. Kocabas N.A., Antonijevic I., Faghel C., Forray C., Kasper S., Lecrubier Y., Linotte S., Massat I., Mendlewicz J., Noro M., et al. Brain-derived neurotrophic factor gene polymorphisms: Influence on treatment response phenotypes of major depressive disorder. Int. Clin. Psychopharmacol. 2011;26:1–10. doi: 10.1097/YIC.0b013e32833d18f8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Xie B., Liu Z., Liu W., Jiang L., Zhang R., Cui D., Zhang Q., Xu S. DNA Methylation and Tag SNPs of the BDNF Gene in Conversion of Amnestic Mild Cognitive Impairment into Alzheimer’s Disease: A Cross-Sectional Cohort Study. J. Alzheimers Dis. 2017;58:263–274. doi: 10.3233/JAD-170007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Ng T., Teo S.M., Yeo H.L., Shwe M., Gan Y.X., Cheung Y.T., Foo K.M., Cham M.T., Lee J.A., Tan Y.P., et al. Brain-derived neurotrophic factor genetic polymorphism (rs6265) is protective against chemotherapy-associated cognitive impairment in patients with early-stage breast cancer. Neuro Oncol. 2016;18:244–251. doi: 10.1093/neuonc/nov162. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 78. Cai Y., Xing L., Yang T., Chai R., Wang J., Bao J., Shen W., Ding S., Chen G. The neurodevelopmental role of dopaminergic signaling in neurological disorders. Neurosci. Lett. 2021;741:135540. doi: 10.1016/j.neulet.2020.135540. [ DOI ] [ PubMed ] [ Google Scholar ]
- 79. Cybulska-Klosowicz A., Laczkowska M., Zakrzewska R., Kaliszewska A. Attentional deficits and altered neuronal activation in medial prefrontal and posterior parietal cortices in mice with reduced dopamine transporter levels. Mol. Cell. Neurosci. 2017;85:82–92. doi: 10.1016/j.mcn.2017.09.004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 80. Mereu M., Contarini G., Buonaguro E.F., Latte G., Manago F., Iasevoli F., de Bartolomeis A., Papaleo F. Dopamine transporter (DAT) genetic hypofunction in mice produces alterations consistent with ADHD but not schizophrenia or bipolar disorder. Neuropharmacology. 2017;121:179–194. doi: 10.1016/j.neuropharm.2017.04.037. [ DOI ] [ PubMed ] [ Google Scholar ]
- 81. Cinque S., Zoratto F., Poleggi A., Leo D., Cerniglia L., Cimino S., Tambelli R., Alleva E., Gainetdinov R.R., Laviola G., et al. Behavioral Phenotyping of Dopamine Transporter Knockout Rats: Compulsive Traits, Motor Stereotypies, and Anhedonia. Front. Psychiatry. 2018;9:43. doi: 10.3389/fpsyt.2018.00043. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 82. Leo D., Sukhanov I., Zoratto F., Illiano P., Caffino L., Sanna F., Messa G., Emanuele M., Esposito A., Dorofeikova M., et al. Pronounced Hyperactivity, Cognitive Dysfunctions, and BDNF Dysregulation in Dopamine Transporter Knock-out Rats. J. Neurosci. 2018;38:1959–1972. doi: 10.1523/JNEUROSCI.1931-17.2018. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 83. Chu C.L., Lee I.H., Chi M.H., Chen K.C., Chen P.S., Yao W.J., Chiu N.T., Yang Y.K. Availability of dopamine transporters and auditory P300 abnormalities in adults with attention-deficit hyperactivity disorder: Preliminary results. CNS Spectr. 2018;23:264–270. doi: 10.1017/S1092852917000049. [ DOI ] [ PubMed ] [ Google Scholar ]
- 84. Pineau G., Villemonteix T., Slama H., Kavec M., Baleriaux D., Metens T., Baijot S., Mary A., Ramoz N., Gorwood P., et al. Dopamine transporter genotype modulates brain activity during a working memory task in children with ADHD. Res. Dev. Disabil. 2019;92:103430. doi: 10.1016/j.ridd.2019.103430. [ DOI ] [ PubMed ] [ Google Scholar ]
- 85. Rommelse N.N., Altink M.E., Arias-Vasquez A., Buschgens C.J., Fliers E., Faraone S.V., Buitelaar J.K., Sergeant J.A., Franke B., Oosterlaan J. A review and analysis of the relationship between neuropsychological measures and DAT1 in ADHD. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2008;147B:1536–1546. doi: 10.1002/ajmg.b.30848. [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. Hong J.H., Hwang I.W., Lim M.H., Kwon H.J., Jin H.J. Genetic associations between ADHD and dopaminergic genes (DAT1 and DRD4) VNTRs in Korean children. Genes Genom. 2018;40:1309–1317. doi: 10.1007/s13258-018-0726-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 87. Stanley A., Chavda K., Subramanian A., Prabhu S.V., Ashavaid T.F. DRD4 and DAT1 VNTR Genotyping in Children with Attention Deficit Hyperactivity Disorder. Indian J. Clin. Biochem. 2017;32:239–242. doi: 10.1007/s12291-016-0587-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 88. Grunblatt E., Werling A.M., Roth A., Romanos M., Walitza S. Association study and a systematic meta-analysis of the VNTR polymorphism in the 3’-UTR of dopamine transporter gene and attention-deficit hyperactivity disorder. J. Neural. Transm. 2019;126:517–529. doi: 10.1007/s00702-019-01998-x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 89. Thursina C., Nurputra D.K., Harahap I.S.K., Harahap N.I.F., Sa’adah N., Wibowo S., Sutarni S., Sadewa A.H., Hanjaya H., Nishio H. Determining the association between polymorphisms of the DAT1 and DRD4 genes with attention deficit hyperactivity disorder in children from Java Island. Neurol. Int. 2020;12:8292. doi: 10.4081/ni.2020.8292. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 90. Bolat H., Ercan E.S., Unsel-Bolat G., Tahillioglu A., Yazici K.U., Bacanli A., Pariltay E., Aygunes Jafari D., Kosova B., Ozgul S., et al. DRD4 genotyping may differentiate symptoms of attention-deficit/hyperactivity disorder and sluggish cognitive tempo. Braz. J. Psychiatry. 2020;42:630–637. doi: 10.1590/1516-4446-2019-0630. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 91. Kuc K., Bielecki M., Racicka-Pawlukiewicz E., Czerwinski M.B., Cybulska-Klosowicz A. The SLC6A3 gene polymorphism is related to the development of attentional functions but not to ADHD. Sci. Rep. 2020;10:6176. doi: 10.1038/s41598-020-63296-x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 92. Ettinger U., Merten N., Kambeitz J. Meta-analysis of the association of the SLC6A3 3’-UTR VNTR with cognition. Neurosci. Biobehav. Rev. 2016;60:72–81. doi: 10.1016/j.neubiorev.2015.09.021. [ DOI ] [ PubMed ] [ Google Scholar ]
- 93. Combita L.M., Voelker P., Abundis-Gutierrez A., Pozuelos J.P., Rueda M.R. Influence of the SLC6A3-DAT1 Gene on Multifaceted Measures of Self-regulation in Preschool Children. Front. Psychol. 2017;8:26. doi: 10.3389/fpsyg.2017.00026. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 94. Areal L.B., Blakely R.D. Neurobehavioral changes arising from early life dopamine signaling perturbations. Neurochem. Int. 2020;137:104747. doi: 10.1016/j.neuint.2020.104747. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 95. Paval D. A Dopamine Hypothesis of Autism Spectrum Disorder. Dev. Neurosci. 2017;39:355–360. doi: 10.1159/000478725. [ DOI ] [ PubMed ] [ Google Scholar ]
- 96. Aguilar-Valles A., Rodrigue B., Matta-Camacho E. Maternal Immune Activation and the Development of Dopaminergic Neurotransmission of the Offspring: Relevance for Schizophrenia and Other Psychoses. Front. Psychiatry. 2020;11:852. doi: 10.3389/fpsyt.2020.00852. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 97. Sonnenschein S.F., Gomes F.V., Grace A.A. Dysregulation of Midbrain Dopamine System and the Pathophysiology of Schizophrenia. Front. Psychiatry. 2020;11:613. doi: 10.3389/fpsyt.2020.00613. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 98. Costa Dias T.G., Wilson V.B., Bathula D.R., Iyer S.P., Mills K.L., Thurlow B.L., Stevens C.A., Musser E.D., Carpenter S.D., Grayson D.S., et al. Reward circuit connectivity relates to delay discounting in children with attention-deficit/hyperactivity disorder. Eur. Neuropsychopharmacol. 2013;23:33–45. doi: 10.1016/j.euroneuro.2012.10.015. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 99. Zhu Y., Jiang X., Ji W. The Mechanism of Cortico-Striato-Thalamo-Cortical Neurocircuitry in Response Inhibition and Emotional Responding in Attention Deficit Hyperactivity Disorder with Comorbid Disruptive Behavior Disorder. Neurosci. Bull. 2018;34:566–572. doi: 10.1007/s12264-018-0214-x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 100. Qiu M.G., Ye Z., Li Q.Y., Liu G.J., Xie B., Wang J. Changes of brain structure and function in ADHD children. Brain Topogr. 2011;24:243–252. doi: 10.1007/s10548-010-0168-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 101. Bonath B., Tegelbeckers J., Wilke M., Flechtner H.H., Krauel K. Regional Gray Matter Volume Differences Between Adolescents With ADHD and Typically Developing Controls: Further Evidence for Anterior Cingulate Involvement. J. Atten. Disord. 2018;22:627–638. doi: 10.1177/1087054715619682. [ DOI ] [ PubMed ] [ Google Scholar ]
- 102. Wyciszkiewicz A., Pawlak M.A., Krawiec K. Cerebellar Volume in Children with Attention-Deficit Hyperactivity Disorder (ADHD) J. Child. Neurol. 2017;32:215–221. doi: 10.1177/0883073816678550. [ DOI ] [ PubMed ] [ Google Scholar ]
- 103. Hoogman M., Muetzel R., Guimaraes J.P., Shumskaya E., Mennes M., Zwiers M.P., Jahanshad N., Sudre G., Wolfers T., Earl E.A., et al. Brain Imaging of the Cortex in ADHD: A Coordinated Analysis of Large-Scale Clinical and Population-Based Samples. Am. J. Psychiatry. 2019;176:531–542. doi: 10.1176/appi.ajp.2019.18091033. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 104. Saute R., Dabbs K., Jones J.E., Jackson D.C., Seidenberg M., Hermann B.P. Brain morphology in children with epilepsy and ADHD. PLoS ONE. 2014;9:e95269. doi: 10.1371/journal.pone.0095269. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 105. Mizuno Y., Kagitani-Shimono K., Jung M., Makita K., Takiguchi S., Fujisawa T.X., Tachibana M., Nakanishi M., Mohri I., Taniike M., et al. Structural brain abnormalities in children and adolescents with comorbid autism spectrum disorder and attention-deficit/hyperactivity disorder. Transl. Psychiatry. 2019;9:332. doi: 10.1038/s41398-019-0679-z. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 106. Bares M., Brunovsky M., Novak T., Kopecek M., Stopkova P., Sos P., Krajca V., Hoschl C. The change of prefrontal QEEG theta cordance as a predictor of response to bupropion treatment in patients who had failed to respond to previous antidepressant treatments. Eur. Neuropsychopharmacol. 2010;20:459–466. doi: 10.1016/j.euroneuro.2010.03.007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 107. Leuchter A.F., McGough J.J., Korb A.S., Hunter A.M., Glaser P.E., Deldar A., Durell T.M., Cook I.A. Neurophysiologic predictors of response to atomoxetine in young adults with attention deficit hyperactivity disorder: A pilot project. J. Psychiatr. Res. 2014;54:11–18. doi: 10.1016/j.jpsychires.2014.03.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 108. Leuchter A.F., Cook I.A., Hunter A., Korb A. Use of clinical neurophysiology for the selection of medication in the treatment of major depressive disorder: The state of the evidence. Clin. EEG Neurosci. 2009;40:78–83. doi: 10.1177/155005940904000207. [ DOI ] [ PubMed ] [ Google Scholar ]
- 109. Hunter A.M., Cook I.A., Abrams M., Leuchter A.F. Neurophysiologic effects of repeated exposure to antidepressant medication: Are brain functional changes during antidepressant administration influenced by learning processes? Med. Hypotheses. 2013;81:1004–1011. doi: 10.1016/j.mehy.2013.09.016. [ DOI ] [ PubMed ] [ Google Scholar ]
- 110. Hunter A.M., Cook I.A., Leuchter A.F. Does prior antidepressant treatment of major depression impact brain function during current treatment? Eur. Neuropsychopharmacol. 2012;22:711–720. doi: 10.1016/j.euroneuro.2012.02.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 111. Clemens B., Menes A., Piros P., Bessenyei M., Altmann A., Jerney J., Kollar K., Rosdy B., Rozsavolgyi M., Steinecker K., et al. Quantitative EEG effects of carbamazepine, oxcarbazepine, valproate, lamotrigine, and possible clinical relevance of the findings. Epilepsy Res. 2006;70:190–199. doi: 10.1016/j.eplepsyres.2006.05.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 112. Loo S.K., Makeig S. Clinical utility of EEG in attention-deficit/hyperactivity disorder: A research update. Neurotherapeutics. 2012;9:569–587. doi: 10.1007/s13311-012-0131-z. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 113. Kim J., Lee Y., Han D., Min K., Kim D., Lee C. The utility of quantitative electroencephalography and Integrated Visual and Auditory Continuous Performance Test as auxiliary tools for the Attention Deficit Hyperactivity Disorder diagnosis. Clin. Neurophysiol. 2015;126:532–540. doi: 10.1016/j.clinph.2014.06.034. [ DOI ] [ PubMed ] [ Google Scholar ]
- 114. Arns M., Conners C.K., Kraemer H.C. A decade of EEG Theta/Beta Ratio Research in ADHD: A meta-analysis. J. Atten. Disord. 2013;17:374–383. doi: 10.1177/1087054712460087. [ DOI ] [ PubMed ] [ Google Scholar ]
- 115. Markovska-Simoska S., Pop-Jordanova N. Quantitative EEG in Children and Adults with Attention Deficit Hyperactivity Disorder: Comparison of Absolute and Relative Power Spectra and Theta/Beta Ratio. Clin. EEG Neurosci. 2017;48:20–32. doi: 10.1177/1550059416643824. [ DOI ] [ PubMed ] [ Google Scholar ]
- 116. Tombor L., Kakuszi B., Papp S., Rethelyi J., Bitter I., Czobor P. Decreased resting gamma activity in adult attention deficit/hyperactivity disorder. World J. Biol. Psychiatry. 2018 doi: 10.1080/15622975.2018.1441547. [ DOI ] [ PubMed ] [ Google Scholar ]
- 117. Acosta M.T. Trastorno por déficit de atención e hiperactividad más allá de la adolescencia ¿tiempo de pensar diferente. Medicina. 2018;78:57–62. [ PubMed ] [ Google Scholar ]
- 118. Kim J.W., Kim S.Y., Choi J.W., Kim K.M., Nam S.H., Min K.J., Lee Y.S., Choi T.Y. Differences in Resting-state Quantitative Electroencephalography Patterns in Attention Deficit/Hyperactivity Disorder with or without Comorbid Symptoms. Clin. Psychopharmacol. Neurosci. 2017;15:138–145. doi: 10.9758/cpn.2017.15.2.138. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 119. Park J.H., Hong J.S., Han D.H., Min K.J., Lee Y.S., Kee B.S., Kim S.M. Comparison of QEEG Findings between Adolescents with Attention Deficit Hyperactivity Disorder (ADHD) without Comorbidity and ADHD Comorbid with Internet Gaming Disorder. J. Korean Med. Sci. 2017;32:514–521. doi: 10.3346/jkms.2017.32.3.514. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 120. Zuluaga-Valencia J.B., Fandiño-Tabares D.C. Comorbilidades asociadas al déficit de atención con hiperactividad. Revista de la Facultad de Medicina. Universidad Nacional de Colombia. 2017;65:61–66. doi: 10.15446/revfacmed.v65n1.57031. [ DOI ] [ Google Scholar ]
- 121. Arns M., Vollebregt M.A., Palmer D., Spooner C., Gordon E., Kohn M., Clarke S., Elliott G.R., Buitelaar J.K. Electroencephalographic biomarkers as predictors of methylphenidate response in attention-deficit/hyperactivity disorder. Eur. Neuropsychopharmacol. 2018;28:881–891. doi: 10.1016/j.euroneuro.2018.06.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 122. Ehlers C.L., Phillips E. EEG low-voltage alpha and alpha power in African American young adults: Relation to family history of alcoholism. Alcohol. Clin. Exp. Res. 2003;27:765–772. doi: 10.1097/01.ALC.0000065439.09492.67. [ DOI ] [ PubMed ] [ Google Scholar ]
- 123. Ehlers C.L., Phillips E., Finnerman G., Gilder D., Lau P., Criado J. P3 components and adolescent binge drinking in Southwest California Indians. Neurotoxicol. Teratol. 2007;29:153–163. doi: 10.1016/j.ntt.2006.11.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 124. Ehlers C.L., Phillips E., Schuckit M.A. EEG alpha variants and alpha power in Hispanic American and white non-Hispanic American young adults with a family history of alcohol dependence. Alcohol. 2004;33:99–106. doi: 10.1016/S0741-8329(04)00098-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 125. Ehlers C.L., Phillips E., Wall T.L., Wilhelmsen K., Schuckit M.A. EEG alpha and level of response to alcohol in Hispanic- and non-Hispanic-American young adults with a family history of alcoholism. J. Stud. Alcohol. 2004;65:301–308. doi: 10.15288/jsa.2004.65.301. [ DOI ] [ PubMed ] [ Google Scholar ]
- 126. Ehlers C.L., Wall T.L., Garcia-Andrade C., Phillips E. Effects of age and parental history of alcoholism on EEG findings in mission Indian children and adolescents. Alcohol. Clin. Exp. Res. 2001;25:672–679. doi: 10.1111/j.1530-0277.2001.tb02266.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 127. Otero G.A. EEG spectral analysis in children with sociocultural handicaps. Int. J. Neurosci. 1994;79:213–220. doi: 10.3109/00207459408986082. [ DOI ] [ PubMed ] [ Google Scholar ]
- 128. Otero G.A., Pliego-Rivero F.B., Fernandez T., Ricardo J. EEG development in children with sociocultural disadvantages: A follow-up study. Clin. Neurophysiol. 2003;114:1918–1925. doi: 10.1016/S1388-2457(03)00173-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 129. Cuzen N.L., Andrew C., Thomas K.G., Stein D.J., Fein G. Absence of P300 reduction in South African treatment-naive adolescents with alcohol dependence. Alcohol. Clin. Exp. Res. 2013;37:40–48. doi: 10.1111/j.1530-0277.2012.01837.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 130. Fein G., Andrew C. Event-related potentials during visual target detection in treatment-naive active alcoholics. Alcohol. Clin. Exp. Res. 2011;35:1171–1179. doi: 10.1111/j.1530-0277.2011.01450.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 131. Herrera-Morales W.V., Ramirez-Lugo L., Santiago-Rodríguez E., Reyes-Lopez J., Núñez-Jaramillo L. Hazardous alcohol consumption and risk of alcohol dependence present different neurophysiological correlates. Rev. Neurol. 2019;68:137–146. [ PubMed ] [ Google Scholar ]
- 132. Brown K.A., Samuel S., Patel D.R. Pharmacologic management of attention deficit hyperactivity disorder in children and adolescents: A review for practitioners. Transl. Pediatr. 2018;7:36–47. doi: 10.21037/tp.2017.08.02. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 133. Cerrillo-Urbina A.J., Garcia-Hermoso A., Pardo-Guijarro M.J., Sanchez-Lopez M., Santos-Gomez J.L., Martinez-Vizcaino V. The Effects of Long-Acting Stimulant and Nonstimulant Medications in Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A Meta-Analysis of Randomized Controlled Trials. J. Child. Adolesc. Psychopharmacol. 2018;28:494–507. doi: 10.1089/cap.2017.0151. [ DOI ] [ PubMed ] [ Google Scholar ]
- 134. Perugi G., Pallucchini A., Rizzato S., Pinzone V., De Rossi P. Current and emerging pharmacotherapy for the treatment of adult attention deficit hyperactivity disorder (ADHD) Expert Opin. Pharmacother. 2019;20:1457–1470. doi: 10.1080/14656566.2019.1618270. [ DOI ] [ PubMed ] [ Google Scholar ]
- 135. Storebo O.J., Pedersen N., Ramstad E., Kielsholm M.L., Nielsen S.S., Krogh H.B., Moreira-Maia C.R., Magnusson F.L., Holmskov M., Gerner T., et al. Methylphenidate for attention deficit hyperactivity disorder (ADHD) in children and adolescents-assessment of adverse events in non-randomised studies. Cochrane Database Syst. Rev. 2018;5:CD012069. doi: 10.1002/14651858.CD012069.pub2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 136. Pievsky M.A., McGrath R.E. Neurocognitive effects of methylphenidate in adults with attention-deficit/hyperactivity disorder: A meta-analysis. Neurosci. Biobehav. Rev. 2018;90:447–455. doi: 10.1016/j.neubiorev.2018.05.012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 137. Zimmer L. Contribution of Clinical Neuroimaging to the Understanding of the Pharmacology of Methylphenidate. Trends Pharmacol. Sci. 2017;38:608–620. doi: 10.1016/j.tips.2017.04.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 138. Savill N.C., Buitelaar J.K., Anand E., Day K.A., Treuer T., Upadhyaya H.P., Coghill D. The efficacy of atomoxetine for the treatment of children and adolescents with attention-deficit/hyperactivity disorder: A comprehensive review of over a decade of clinical research. CNS Drugs. 2015;29:131–151. doi: 10.1007/s40263-014-0224-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 139. Childress A.C. A critical appraisal of atomoxetine in the management of ADHD. Ther. Clin. Risk Manag. 2016;12:27–39. doi: 10.2147/TCRM.S59270. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 140. Meridor K., Levy Y. Systemic sclerosis induced by CNS stimulants for ADHD: A case series and review of the literature. Autoimmun. Rev. 2020;19:102439. doi: 10.1016/j.autrev.2019.102439. [ DOI ] [ PubMed ] [ Google Scholar ]
- 141. Reed V.A., Buitelaar J.K., Anand E., Day K.A., Treuer T., Upadhyaya H.P., Coghill D.R., Kryzhanovskaya L.A., Savill N.C. The Safety of Atomoxetine for the Treatment of Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A Comprehensive Review of Over a Decade of Research. CNS Drugs. 2016;30:603–628. doi: 10.1007/s40263-016-0349-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 142. Clemow D.B., Bushe C., Mancini M., Ossipov M.H., Upadhyaya H. A review of the efficacy of atomoxetine in the treatment of attention-deficit hyperactivity disorder in children and adult patients with common comorbidities. Neuropsychiatr. Dis. Treat. 2017;13:357–371. doi: 10.2147/NDT.S115707. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 143. Hutchison S.L., Ghuman J.K., Ghuman H.S., Karpov I., Schuster J.M. Efficacy of atomoxetine in the treatment of attention-deficit hyperactivity disorder in patients with common comorbidities in children, adolescents and adults: A review. Ther. Adv. Psychopharmacol. 2016;6:317–334. doi: 10.1177/2045125316647686. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 144. Yang R., Li R., Gao W., Zhao Z. Tic Symptoms Induced by Atomoxetine in Treatment of ADHD: A Case Report and Literature Review. J. Dev. Behav. Pediatr. 2017;38:151–154. doi: 10.1097/DBP.0000000000000371. [ DOI ] [ PubMed ] [ Google Scholar ]
- 145. Fay T.B., Alpert M.A. Cardiovascular Effects of Drugs Used to Treat Attention-Deficit/Hyperactivity Disorder Part 2: Impact on Cardiovascular Events and Recommendations for Evaluation and Monitoring. Cardiol. Rev. 2019;27:173–178. doi: 10.1097/CRD.0000000000000234. [ DOI ] [ PubMed ] [ Google Scholar ]
- 146. Catala-Lopez F., Hutton B., Nunez-Beltran A., Page M.J., Ridao M., Macias Saint-Gerons D., Catala M.A., Tabares-Seisdedos R., Moher D. The pharmacological and non-pharmacological treatment of attention deficit hyperactivity disorder in children and adolescents: A systematic review with network meta-analyses of randomised trials. PLoS ONE. 2017;12:e0180355. doi: 10.1371/journal.pone.0180355. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 147. Wang Y., Zheng Y., Du Y., Song D.H., Shin Y.J., Cho S.C., Kim B.N., Ahn D.H., Marquez-Caraveo M.E., Gao H., et al. Atomoxetine versus methylphenidate in paediatric outpatients with attention deficit hyperactivity disorder: A randomized, double-blind comparison trial. Aust. N. Z. J. Psychiatry. 2007;41:222–230. doi: 10.1080/00048670601057767. [ DOI ] [ PubMed ] [ Google Scholar ]
- 148. Garg J., Arun P., Chavan B.S. Comparative short term efficacy and tolerability of methylphenidate and atomoxetine in attention deficit hyperactivity disorder. Indian Pediatr. 2014;51:550–554. doi: 10.1007/s13312-014-0445-5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 149. Holmskov M., Storebo O.J., Moreira-Maia C.R., Ramstad E., Magnusson F.L., Krogh H.B., Groth C., Gillies D., Zwi M., Skoog M., et al. Gastrointestinal adverse events during methylphenidate treatment of children and adolescents with attention deficit hyperactivity disorder: A systematic review with meta-analysis and Trial Sequential Analysis of randomised clinical trials. PLoS ONE. 2017;12:e0178187. doi: 10.1371/journal.pone.0178187. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 150. Cortese S., Panei P., Arcieri R., Germinario E.A., Capuano A., Margari L., Chiarotti F., Curatolo P. Safety of Methylphenidate and Atomoxetine in Children with Attention-Deficit/Hyperactivity Disorder (ADHD): Data from the Italian National ADHD Registry. CNS Drugs. 2015;29:865–877. doi: 10.1007/s40263-015-0266-7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 151. Loureiro-Vieira S., Costa V.M., de Lourdes Bastos M., Carvalho F., Capela J.P. Methylphenidate effects in the young brain: Friend or foe? Int. J. Dev. Neurosci. 2017;60:34–47. doi: 10.1016/j.ijdevneu.2017.04.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 152. Krinzinger H., Hall C.L., Groom M.J., Ansari M.T., Banaschewski T., Buitelaar J.K., Carucci S., Coghill D., Danckaerts M., Dittmann R.W., et al. Neurological and psychiatric adverse effects of long-term methylphenidate treatment in ADHD: A map of the current evidence. Neurosci. Biobehav. Rev. 2019;107:945–968. doi: 10.1016/j.neubiorev.2019.09.023. [ DOI ] [ PubMed ] [ Google Scholar ]
- 153. Wong I.C.K., Banaschewski T., Buitelaar J., Cortese S., Dopfner M., Simonoff E., Coghill D., European A.G.G. Emerging challenges in pharmacotherapy research on attention-deficit hyperactivity disorder-outcome measures beyond symptom control and clinical trials. Lancet Psychiatry. 2019;6:528–537. doi: 10.1016/S2215-0366(19)30096-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 154. Coghill D. Debate: Are Stimulant Medications for Attention-Deficit/Hyperactivity Disorder Effective in the Long Term? (For) J. Am. Acad. Child. Adolesc. Psychiatry. 2019;58:938–939. doi: 10.1016/j.jaac.2019.07.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 155. Cortese S. Debate: Are Stimulant Medications for Attention-Deficit/Hyperactivity Disorder Effective in the Long Term? J. Am. Acad. Child. Adolesc. Psychiatry. 2019;58:936. doi: 10.1016/j.jaac.2019.04.029. [ DOI ] [ PubMed ] [ Google Scholar ]
- 156. Swanson J.M. Debate: Are Stimulant Medications for Attention-Deficit/Hyperactivity Disorder Effective in the Long Term? (Against) J. Am. Acad. Child. Adolesc. Psychiatry. 2019;58:936–938. doi: 10.1016/j.jaac.2019.07.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 157. Elsayed N.A., Yamamoto K.M., Froehlich T.E. Genetic Influence on Efficacy of Pharmacotherapy for Pediatric Attention-Deficit/Hyperactivity Disorder: Overview and Current Status of Research. CNS Drugs. 2020;34:389–414. doi: 10.1007/s40263-020-00702-y. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 158. Chiarenza G.A., Chabot R., Isenhart R., Montaldi L., Chiarenza M.P., Torto M.G., Prichep L.S. The quantified EEG characteristics of responders and non-responders to long-term treatment with atomoxetine in children with attention deficit hyperactivity disorders. Int. J. Psychophysiol. 2016;104:44–52. doi: 10.1016/j.ijpsycho.2016.04.004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 159. Spencer T., Biederman J., Wilens T., Harding M., O’Donnell D., Griffin S. Pharmacotherapy of attention-deficit hyperactivity disorder across the life cycle. J. Am. Acad. Child. Adolesc. Psychiatry. 1996;35:409–432. doi: 10.1097/00004583-199604000-00008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 160. Ogrim G., Kropotov J.D. Predicting Clinical Gains and Side Effects of Stimulant Medication in Pediatric Attention-Deficit/Hyperactivity Disorder by Combining Measures From qEEG and ERPs in a Cued GO/NOGO Task. Clin. EEG Neurosci. 2019;50:34–43. doi: 10.1177/1550059418782328. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 161. Buoli M., Serati M., Cahn W. Alternative pharmacological strategies for adult ADHD treatment: A systematic review. Expert Rev. Neurother. 2016;16:131–144. doi: 10.1586/14737175.2016.1135735. [ DOI ] [ PubMed ] [ Google Scholar ]
- 162. Zwi M., Jones H., Thorgaard C., York A., Dennis J.A. Parent training interventions for Attention Deficit Hyperactivity Disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst. Rev. 2011 doi: 10.1002/14651858.CD003018.pub3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 163. Chacko A., Bedard A.V., Marks D., Gopalan G., Feirsen N., Uderman J., Chimiklis A., Heber E., Cornwell M., Anderson L., et al. Sequenced neurocognitive and behavioral parent training for the treatment of ADHD in school-age children. Child. Neuropsychol. 2018;24:427–450. doi: 10.1080/09297049.2017.1282450. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 164. Fosco W.D., Sarver D.E., Kofler M.J., Aduen P.A. Parent and child neurocognitive functioning predict response to behavioral parent training for youth with ADHD. Atten. Defic. Hyperact. Disord. 2018;10:285–295. doi: 10.1007/s12402-018-0259-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 165. Ciesielski H.A., Loren R.E.A., Tamm L. Behavioral Parent Training for ADHD Reduces Situational Severity of Child Noncompliance and Related Parental Stress. J. Atten. Disord. 2020;24:758–767. doi: 10.1177/1087054719843181. [ DOI ] [ PubMed ] [ Google Scholar ]
- 166. Jensen C.M., Amdisen B.L., Jorgensen K.J., Arnfred S.M. Cognitive behavioural therapy for ADHD in adults: Systematic review and meta-analyses. Atten. Defic. Hyperact. Disord. 2016;8:3–11. doi: 10.1007/s12402-016-0188-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 167. Knouse L.E., Teller J., Brooks M.A. Meta-analysis of cognitive-behavioral treatments for adult ADHD. J. Consult. Clin. Psychol. 2017;85:737–750. doi: 10.1037/ccp0000216. [ DOI ] [ PubMed ] [ Google Scholar ]
- 168. Lopez P.L., Torrente F.M., Ciapponi A., Lischinsky A.G., Cetkovich-Bakmas M., Rojas J.I., Romano M., Manes F.F. Cognitive-behavioural interventions for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst. Rev. 2018;3:CD010840. doi: 10.1002/14651858.CD010840.pub2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 169. Lambez B., Harwood-Gross A., Golumbic E.Z., Rassovsky Y. Non-pharmacological interventions for cognitive difficulties in ADHD: A systematic review and meta-analysis. J. Psychiatr. Res. 2020;120:40–55. doi: 10.1016/j.jpsychires.2019.10.007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 170. Nimmo-Smith V., Merwood A., Hank D., Brandling J., Greenwood R., Skinner L., Law S., Patel V., Rai D. Non-pharmacological interventions for adult ADHD: A systematic review. Psychol. Med. 2020;50:529–541. doi: 10.1017/S0033291720000069. [ DOI ] [ PubMed ] [ Google Scholar ]
- 171. Pan M.R., Huang F., Zhao M.J., Wang Y.F., Wang Y.F., Qian Q.J. A comparison of efficacy between cognitive behavioral therapy (CBT) and CBT combined with medication in adults with attention-deficit/hyperactivity disorder (ADHD) Psychiatry Res. 2019;279:23–33. doi: 10.1016/j.psychres.2019.06.040. [ DOI ] [ PubMed ] [ Google Scholar ]
- 172. Modesto-Lowe V., Farahmand P., Chaplin M., Sarro L. Does mindfulness meditation improve attention in attention deficit hyperactivity disorder? World J. Psychiatry. 2015;5:397–403. doi: 10.5498/wjp.v5.i4.397. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 173. Lee C.S.C., Ma M.T., Ho H.Y., Tsang K.K., Zheng Y.Y., Wu Z.Y. The Effectiveness of Mindfulness-Based Intervention in Attention on Individuals with ADHD: A Systematic Review. Hong Kong J. Occup. Ther. 2017;30:33–41. doi: 10.1016/j.hkjot.2017.05.001. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 174. Vancampfort D., Stubbs B., Van Damme T., Smith L., Hallgren M., Schuch F., Deenik J., Rosenbaum S., Ashdown-Franks G., Mugisha J., et al. The efficacy of meditation-based mind-body interventions for mental disorders: A meta-review of 17 meta-analyses of randomized controlled trials. J. Psychiatr. Res. 2020;134:181–191. doi: 10.1016/j.jpsychires.2020.12.048. [ DOI ] [ PubMed ] [ Google Scholar ]
- 175. Aadil M., Cosme R.M., Chernaik J. Mindfulness-Based Cognitive Behavioral Therapy as an Adjunct Treatment of Attention Deficit Hyperactivity Disorder in Young Adults: A Literature Review. Cureus. 2017;9:e1269. doi: 10.7759/cureus.1269. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 176. Evans S., Ling M., Hill B., Rinehart N., Austin D., Sciberras E. Systematic review of meditation-based interventions for children with ADHD. Eur. Child Adolesc. Psychiatry. 2018;27:9–27. doi: 10.1007/s00787-017-1008-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 177. Nicastro R., Jermann F., Bluteau Blin S., Waeber C., Perroud N. Mindfulness Training for Adults with Attention-Deficit/Hyperactivity Disorder: Implementation of Mindful Awareness Practices in a French-Speaking Attention-Deficit/Hyperactivity Disorder Unit. J. Altern. Complement. Med. 2020 doi: 10.1089/acm.2020.0216. [ DOI ] [ PubMed ] [ Google Scholar ]
- 178. Santonastaso O., Zaccari V., Crescentini C., Fabbro F., Capurso V., Vicari S., Menghini D. Clinical Application of Mindfulness-Oriented Meditation: A Preliminary Study in Children with ADHD. Int. J. Environ. Res. Public Health. 2020;17:6916. doi: 10.3390/ijerph17186916. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 179. Muratori P., Conversano C., Levantini V., Masi G., Milone A., Villani S., Bogels S., Gemignani A. Exploring the Efficacy of a Mindfulness Program for Boys With Attention-Deficit Hyperactivity Disorder and Oppositional Defiant Disorder. J. Atten. Disord. 2020 doi: 10.1177/1087054720915256. [ DOI ] [ PubMed ] [ Google Scholar ]
- 180. Van Doren J., Heinrich H., Bezold M., Reuter N., Kratz O., Horndasch S., Berking M., Ros T., Gevensleben H., Moll G.H., et al. Theta/beta neurofeedback in children with ADHD: Feasibility of a short-term setting and plasticity effects. Int. J. Psychophysiol. 2017;112:80–88. doi: 10.1016/j.ijpsycho.2016.11.004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 181. Ros T., Baars B., Lanius R.A., Vuilleumier P. Tuning pathological brain oscillations with neurofeedback: A systems neuroscience framework. Front. Hum. Neurosci. 2014;8:1008. doi: 10.3389/fnhum.2014.01008. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 182. Ros T., Munneke M.A., Ruge D., Gruzelier J.H., Rothwell J.C. Endogenous control of waking brain rhythms induces neuroplasticity in humans. Eur. J. Neurosci. 2010;31:770–778. doi: 10.1111/j.1460-9568.2010.07100.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 183. Ros T., Theberge J., Frewen P.A., Kluetsch R., Densmore M., Calhoun V.D., Lanius R.A. Mind over chatter: Plastic up-regulation of the fMRI salience network directly after EEG neurofeedback. Neuroimage. 2013;65:324–335. doi: 10.1016/j.neuroimage.2012.09.046. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 184. Arns M., Heinrich H., Strehl U. Evaluation of neurofeedback in ADHD: The long and winding road. Biol. Psychol. 2014;95:108–115. doi: 10.1016/j.biopsycho.2013.11.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 185. Enriquez-Geppert S., Smit D., Pimenta M.G., Arns M. Neurofeedback as a Treatment Intervention in ADHD: Current Evidence and Practice. Curr. Psychiatry Rep. 2019;21:46. doi: 10.1007/s11920-019-1021-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 186. Bussalb A., Congedo M., Barthelemy Q., Ojeda D., Acquaviva E., Delorme R., Mayaud L. Clinical and Experimental Factors Influencing the Efficacy of Neurofeedback in ADHD: A Meta-Analysis. Front. Psychiatry. 2019;10:35. doi: 10.3389/fpsyt.2019.00035. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 187. Van Doren J., Arns M., Heinrich H., Vollebregt M.A., Strehl U., Loo S.K. Sustained effects of neurofeedback in ADHD: A systematic review and meta-analysis. Eur. Child. Adolesc. Psychiatry. 2019;28:293–305. doi: 10.1007/s00787-018-1121-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 188. Cortese S., Ferrin M., Brandeis D., Holtmann M., Aggensteiner P., Daley D., Santosh P., Simonoff E., Stevenson J., Stringaris A., et al. Neurofeedback for Attention-Deficit/Hyperactivity Disorder: Meta-Analysis of Clinical and Neuropsychological Outcomes From Randomized Controlled Trials. J. Am. Acad. Child. Adolesc. Psychiatry. 2016;55:444–455. doi: 10.1016/j.jaac.2016.03.007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 189. Yan L., Wang S., Yuan Y., Zhang J. Effects of neurofeedback versus methylphenidate for the treatment of ADHD: Systematic review and meta-analysis of head-to-head trials. Evid. Based Ment. Health. 2019;22:111–117. doi: 10.1136/ebmental-2019-300088. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 190. Riesco-Matias P., Yela-Bernabe J.R., Crego A., Sanchez-Zaballos E. What Do Meta-Analyses Have to Say About the Efficacy of Neurofeedback Applied to Children with ADHD? Review of Previous Meta-Analyses and a New Meta-Analysis. J. Atten. Disord. 2019 doi: 10.1177/1087054718821731. [ DOI ] [ PubMed ] [ Google Scholar ]
- 191. Razoki B. Neurofeedback versus psychostimulants in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: A systematic review. Neuropsychiatr. Dis. Treat. 2018;14:2905–2913. doi: 10.2147/NDT.S178839. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 192. Mohagheghi A., Amiri S., Moghaddasi Bonab N., Chalabianloo G., Noorazar S.G., Tabatabaei S.M., Farhang S. A Randomized Trial of Comparing the Efficacy of Two Neurofeedback Protocols for Treatment of Clinical and Cognitive Symptoms of ADHD: Theta Suppression/Beta Enhancement and Theta Suppression/Alpha Enhancement. Biomed. Res. Int. 2017;2017:3513281. doi: 10.1155/2017/3513281. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 193. Dobrakowski P., Lebecka G. Individualized Neurofeedback Training May Help Achieve Long-Term Improvement of Working Memory in Children With ADHD. Clin. EEG Neurosci. 2020;51:94–101. doi: 10.1177/1550059419879020. [ DOI ] [ PubMed ] [ Google Scholar ]
- 194. Schonenberg M., Wiedemann E., Schneidt A., Scheeff J., Logemann A., Keune P.M., Hautzinger M. Neurofeedback, sham neurofeedback, and cognitive-behavioural group therapy in adults with attention-deficit hyperactivity disorder: A triple-blind, randomised, controlled trial. Lancet Psychiatry. 2017;4:673–684. doi: 10.1016/S2215-0366(17)30291-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 195. Neurofeedback Collaborative G. Double-Blind Placebo-Controlled Randomized Clinical Trial of Neurofeedback for Attention-Deficit/Hyperactivity Disorder With 13-Month Follow-up. J. Am. Acad. Child. Adolesc. Psychiatry. 2020 doi: 10.1016/j.jaac.2020.07.906. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 196. Janssen T.W.P., Gelade K., Bink M., van Mourik R., Twisk J.W.R., Maras A., Oosterlaan J. Long-term effects of theta/beta neurofeedback on EEG power spectra in children with attention deficit hyperactivity disorder. Clin. Neurophysiol. 2020;131:1332–1341. doi: 10.1016/j.clinph.2020.02.020. [ DOI ] [ PubMed ] [ Google Scholar ]
- 197. Pakdaman F., Irani F., Tajikzadeh F., Jabalkandi S.A. The efficacy of Ritalin in ADHD children under neurofeedback training. Neurol. Sci. 2018;39:2071–2078. doi: 10.1007/s10072-018-3539-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 198. Moreno-Garcia I., Meneres-Sancho S., Camacho-Vara de Rey C., Servera M. A Randomized Controlled Trial to Examine the Posttreatment Efficacy of Neurofeedback, Behavior Therapy, and Pharmacology on ADHD Measures. J. Atten. Disord. 2019;23:374–383. doi: 10.1177/1087054717693371. [ DOI ] [ PubMed ] [ Google Scholar ]
- 199. Gelade K., Bink M., Janssen T.W., van Mourik R., Maras A., Oosterlaan J. An RCT into the effects of neurofeedback on neurocognitive functioning compared to stimulant medication and physical activity in children with ADHD. Eur. Child. Adolesc. Psychiatry. 2017;26:457–468. doi: 10.1007/s00787-016-0902-x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 200. Rosi E., Grazioli S., Villa F.M., Mauri M., Gazzola E., Pozzi M., Molteni M., Nobile M. Use of Non-Pharmacological Supplementations in Children and Adolescents with Attention Deficit/Hyperactivity Disorder: A Critical Review. Nutrients. 2020;12:1573. doi: 10.3390/nu12061573. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 201. Noorazar S.G., Malek A., Aghaei S.M., Yasamineh N., Kalejahi P. The efficacy of zinc augmentation in children with attention deficit hyperactivity disorder under treatment with methylphenidate: A randomized controlled trial. Asian J. Psychiatr. 2020;48:101868. doi: 10.1016/j.ajp.2019.101868. [ DOI ] [ PubMed ] [ Google Scholar ]
- 202. Aldemir R., Demirci E., Bayram A.K., Canpolat M., Ozmen S., Per H., Tokmakci M. Evaluation of Two Types of Drug Treatment with QEEG in Children with ADHD. Transl. Neurosci. 2018;9:106–116. doi: 10.1515/tnsci-2018-0017. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 203. Surmeli T., Ertem A., Eralp E., Kos I.H. Schizophrenia and the efficacy of qEEG-guided neurofeedback treatment: A clinical case series. Clin. EEG Neurosci. 2012;43:133–144. doi: 10.1177/1550059411429531. [ DOI ] [ PubMed ] [ Google Scholar ]
- 204. Surmeli T., Ertem A. Obsessive compulsive disorder and the efficacy of qEEG-guided neurofeedback treatment: A case series. Clin. EEG Neurosci. 2011;42:195–201. doi: 10.1177/155005941104200310. [ DOI ] [ PubMed ] [ Google Scholar ]
- 205. Walker J.E. QEEG-guided neurofeedback for recurrent migraine headaches. Clin. EEG Neurosci. 2011;42:59–61. doi: 10.1177/155005941104200112. [ DOI ] [ PubMed ] [ Google Scholar ]
- 206. Surmeli T., Eralp E., Mustafazade I., Kos H., Ozer G.E., Surmeli O.H. Quantitative EEG Neurometric Analysis-Guided Neurofeedback Treatment in Dementia: 20 Cases. How Neurometric Analysis Is Important for the Treatment of Dementia and as a Biomarker? Clin. EEG Neurosci. 2016;47:118–133. doi: 10.1177/1550059415590750. [ DOI ] [ PubMed ] [ Google Scholar ]
- 207. Fernandez T., Herrera W., Harmony T., Diaz-Comas L., Santiago E., Sanchez L., Bosch J., Fernandez-Bouzas A., Otero G., Ricardo-Garcell J., et al. EEG and behavioral changes following neurofeedback treatment in learning disabled children. Clin. Electroencephalogr. 2003;34:145–152. doi: 10.1177/155005940303400308. [ DOI ] [ PubMed ] [ Google Scholar ]
- 208. Becerra J., Fernandez T., Harmony T., Caballero M.I., Garcia F., Fernandez-Bouzas A., Santiago-Rodriguez E., Prado-Alcala R.A. Follow-up study of learning-disabled children treated with neurofeedback or placebo. Clin. EEG Neurosci. 2006;37:198–203. doi: 10.1177/155005940603700307. [ DOI ] [ PubMed ] [ Google Scholar ]
- 209. Arns M., Drinkenburg W., Leon Kenemans J. The effects of QEEG-informed neurofeedback in ADHD: An open-label pilot study. Appl. Psychophysiol. Biofeedback. 2012;37:171–180. doi: 10.1007/s10484-012-9191-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 210. Krepel N., Egtberts T., Sack A.T., Heinrich H., Ryan M., Arns M. A multicenter effectiveness trial of QEEG-informed neurofeedback in ADHD: Replication and treatment prediction. Neuroimage Clin. 2020;28:102399. doi: 10.1016/j.nicl.2020.102399. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 211. Ligezka A.N., Sonmez A.I., Corral-Frias M.P., Golebiowski R., Lynch B., Croarkin P.E., Romanowicz M. A systematic review of microbiome changes and impact of probiotic supplementation in children and adolescents with neuropsychiatric disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2020 doi: 10.1016/j.pnpbp.2020.110187. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 212. Boonchooduang N., Louthrenoo O., Chattipakorn N., Chattipakorn S.C. Possible links between gut-microbiota and attention-deficit/hyperactivity disorders in children and adolescents. Eur. J. Nutr. 2020;59:3391–3403. doi: 10.1007/s00394-020-02383-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 213. Hiergeist A., Gessner J., Gessner A. Current Limitations for the Assessment of the Role of the Gut Microbiome for Attention Deficit Hyperactivity Disorder (ADHD) Front. Psychiatry. 2020;11:623. doi: 10.3389/fpsyt.2020.00623. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 214. Mathee K., Cickovski T., Deoraj A., Stollstorff M., Narasimhan G. The gut microbiome and neuropsychiatric disorders: Implications for attention deficit hyperactivity disorder (ADHD) J. Med. Microbiol. 2020;69:14–24. doi: 10.1099/jmm.0.001112. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (467.2 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Expert Review
- Open access
- Published: 08 June 2024
Improving the efficacy and effectiveness of evidence-based psychosocial interventions for attention-deficit/hyperactivity disorder (ADHD) in children and adolescents
- Anil Chacko ORCID: orcid.org/0000-0002-3275-4726 1 ,
- Brittany M. Merrill 2 ,
- Michael J. Kofler ORCID: orcid.org/0000-0002-8604-3647 3 &
- Gregory A. Fabiano 2
Translational Psychiatry volume 14 , Article number: 244 ( 2024 ) Cite this article
6658 Accesses
1 Altmetric
Metrics details
- Human behaviour
Attention-deficit/hyperactivity disorder (ADHD) is a prevalent, chronic, and impairing mental health disorder of childhood. Decades of empirical research has established a strong evidence-based intervention armamentarium for ADHD; however, limitations exist in regards to efficacy and effectiveness of these interventions. We provide an overview of select evidence-based interventions for children and adolescents, highlighting potential approaches to further improving the efficacy and effectiveness of these interventions. We conclude with broader recommendations for interventions, including considerations to moderators and under-explored intervention target areas as well as avenues to improve access and availability of evidence-based interventions through leveraging underutilized workforces and leveraging technology.
Similar content being viewed by others

RETRACTED ARTICLE: Is homeopathy effective for attention deficit and hyperactivity disorder? A meta-analysis

Medical conditions and Attention-Deficit/Hyperactivity Disorder symptoms from early childhood to adolescence
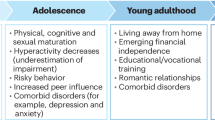
Perspectives on parental support of attention deficit hyperactivity disorder self-management at the transition to adulthood
Evidence-based treatments for adhd - an overview.
Multiple groups, committees, and professional organizations have provided the field with recommendations for evidence-based treatment approaches for ADHD. There is clear consensus across these recommendations that pharmacological treatments, notably stimulant medication, psychosocial treatments, and a combination of these two approaches have the strongest evidence base. Table 1 provides a brief overview of the major conclusions of each guideline for the treatment of ADHD in children. It is clearly recommended that families should receive psychoeducation regarding ADHD, and that the evidence-based psychosocial treatments are behavioral parent training (BPT), behavioral interventions in classroom and peer settings, and organizational skills training [ 1 , 2 , 3 , 4 , 5 ].
There are inconsistencies among the guidelines that make broad statements of consensus difficult. For instance, there are differences in precision in recommendations for psychosocial treatments, with some very broad in scope [ 6 ] compared to others with more precise recommendations regarding particular treatment types (e.g., BPT [ 2 ]) and particular populations (e.g., children under six; [ 5 ]). Broad suggestions of seeking “psychological” or “educational” treatment is unhelpful in some guidelines and practice parameters, as there are many approaches that fall under this category and some are clearly efficacious whereas other approaches commonly deployed do not have evidence of efficacy for ADHD [ 1 , 2 , 3 , 4 ]. There are also differences in the strength of recommendations, with more contemporary guidelines emphasizing multimodal treatments more so than older guidelines. However, perhaps most notably, there is not clear consensus among the recommendations on the best sequence or combination of treatments for ADHD, even though this is a key question for most families pursuing treatment for ADHD. It is also important to note that most guidelines focus on proximal ADHD treatment – as ADHD is now conceptualized as a life-course persistent disorder [ 7 ], treatment efforts will need to be protracted across time and appropriate for evolving developmental levels.
Efforts at improving efficacy and effectiveness of psychosocial intervention for ADHD: what do we know and where do we go?
Given the prominent role of psychosocial, primarily behavioral interventions, for ADHD, we highlight the evidence for several of these key interventions, integrating the literature on improving efficacy and effectiveness of these interventions. We also discuss digital therapeutics given the explosion in its availability and purported efficacy for children with ADHD. Following this, we close with potential broad future directions for psychosocial treatments for children with ADHD.
Behavioral parent training
Behavioral parent training (BPT) is likely the most well-studied psychosocial intervention for children’s mental health disorders, including for ADHD [ 8 ]. It serves as the first line intervention approach for younger children with ADHD and is an integral part of comprehensive intervention approaches for school-age children with ADHD. Importantly, BPT is less studied in adolescents with ADHD. Although parenting is not etiological to ADHD, there are clear reasons to focus on parenting when supporting a child with ADHD. Of primary importance is that raising a child with ADHD is stressful, and not surprisingly, elicits ineffectual parenting practices (e.g., inconsistent, harsh, lax, overreactive, less responsive). As a result, parents often have lower parenting efficacy/competence, higher levels of coercive management practices, utilize maladaptive coping strategies (e.g., increased use of alcohol), and have more negative attributions/perceptions of their child [ 8 ]. These parent-level challenges can be addressed, in part, by supporting parents to utilize more proactive and effective parenting practices which can help improve functioning for themselves and ultimately their children. Importantly, the most common comorbidities with ADHD, Oppositional Defiant Disorder [ODD] and Conduct Disorder (CD) are best treated with BPT—making BPT an essential treatment for the most common disruptive behavior disorders in childhood [ 8 ].
BPT is based on operant-conditioning and social learning theories, with techniques that focus on antecedents (e.g., effective instructions, rules) and consequences (e.g., active ignoring, time-out from positive reinforcement) of behaviors. This core content is delivered in a flexible manner with varying formats (e.g., group, individual) durations (brief vs longer), with or without child involvement, delivery (e.g., with or without video-based learning). Moreover, over the past two decades, there have been efforts at tailoring BPT to meet the needs of specific populations (e.g., single mothers, fathers; Latine; [ 9 , 10 , 11 , 12 ]). These BPT programs, often referred to as “homegrown” BPT as compared to commercialized BPT programs (those that have been more extensively developed, manualized and are commercially available; e.g., Defiant Children [ 13 ]) retain the core content of traditional BPT but have modifications to format or additional content that are based on the needs of the targeted populations. Overall, commercialized BPT and homegrown BPT have been found to be effective in improving the functioning of children with ADHD and their parents [ 14 , 15 , 16 ]. A recent meta-analysis also suggests sustained benefits of BPT over the course of a year on child ADHD symptoms, parenting behavior, parenting sense of competence and parental mental health [ 17 ]. The significance of BPT should be, however, put into a broader context to appreciate the clinical benefits of this intervention. While multiple randomized controlled trials have established the statistical significance of BPT for ADHD, the effect size for BPT ranges from small to medium effects, depending upon the outcome [ 18 ]. This means that for many outcomes, the effect sizes would be “visible to the naked eye of a careful observer” [ 19 ]. While there is limited data, only a significant minority of children are “normalized” following BPT [ 15 ]. Collectively, a more nuanced perspective on BPT for ADHD suggests that it is an evidence-based intervention that can result in visible improvements on key outcomes. There is room, however, to improve the potency of BPT. The implications of the findings reported above suggest several broad areas for further investigation. First is to increase access to BPT given the benefits of the intervention. Wolraich et al. [ 20 ] note that there is a lack of an adequate pool of behavioral and mental health specialists who are available to provide evidence-based psychosocial treatments for ADHD, including BPT. National data suggest that the majority of youth with ADHD are receiving no treatment, even when identified, and the lack of BPT treatment is most pronounced in young children with ADHD [ 21 ]. Efforts at utilizing technology to increase the workforce offers novel and promising approaches to address this issue [ 22 ].
A second area is to increase the potency of BPT. We believe there are multiple ways to achieve this goal, with the most apparent being improving the extent to which parents fully engage in BPT, given the relation between increased engagement and improved potency of outcomes [ 23 ]. It is common for families of children with ADHD, even those who have enrolled in BPT, to not initiate treatment or drop out of BPT prior to completion [ 9 , 23 ]. Given this, there have been notable efforts at improving engagement to BPT through addressing perceptual (e.g., expectations about BPT), practical (e.g., transportation) and cultural barriers to treatment prior to BPT [ 10 , 24 ] as well as during BPT [ 25 ]. Given that engagement challenges often involve practical barriers (e.g., transportation, child care, fixed appointment times), there has been efforts at increasing access through reducing these barriers such as providing BPT through mobile applications [ 26 ], web-based platforms [ 27 ] and telehealth delivery [ 28 , 29 ]. These efforts have led to improved engagement and associated outcomes for families, beyond traditional BPT [ 30 ]. Engagement with BPT remains an important area of research, particularly the extent to which these enhancements to BPT can be readily applied in routine settings [ 25 , 31 , 32 ], an understudied empirical question.
A second and meaningful line of research to improve the potency of BPT has been focused on improving specificity of BPT content by translating contemporary theories of ADHD into refinements to BPT. Van der Oord and Tripp [ 33 ]), utilizing contemporary motivational reinforcement-based theories of ADHD, suggest that given altered reinforcement sensitivity in ADHD, rewards and punishment should be judiciously provided. As an example, they note evidence that while mild negative punishment (e.g., response-cost, time-out from positive reinforcement) improves on-task behavior in children with ADHD, mild punishment can also lead to more errors on tasks, increased emotionality in children with ADHD, missed learning opportunities, and lack of task persistence [ 34 , 35 ]. These authors note caution in the use of punishment, especially positive punishment (e.g., verbal reprimands), with children with ADHD. Rather, there should be a focus on rewarding alternative adaptive behaviors to reduce the need to use punishment. These theory-driven considerations to adapting BPT are important, yet empirically understudied. As such, the extent to which these ADHD-theory-adapted BPT results in improved outcomes relative to standard BPT is not known. Importantly, however, some efforts in this area have resulted in little difference for ADHD-adapted BPT relative to standard BPT. As an example, in an RCT, the New Forest Parenting Program (NFPP), which was developed to address underlying mechanisms of ADHD (self-regulatory and cognitive problems [ 36 ] was found to be no better than a standard BPT program and in some areas less effective (e.g., parental stress, parenting behavior, parent reports of ADHD symptoms at follow-up) for preschool children with ADHD [ 37 ]. These data suggest the importance of rigorously evaluating novel approaches that are considered improvements to BPT to well-established traditional BPT for ADHD.
Overall, the efficacy of BPT suggests that this should be first-line intervention approach for children with ADHD, with significant and noticeable effects of BPT on both parent- and child-level outcomes with maintenance of gains over the course of a year. This statement comes with the caveat that there is room for improvement in the potency of BPT. As we will discuss in the future directions section below, greater attention must be given to dissemination of BPT (and all psychosocial interventions for ADHD) within routine systems of care and evaluation of the effectiveness of these interventions alone and in combination when delivered within these systems.
Behavioral classroom management
ADHD is largely defined by challenges in settings such as schools where behavioral expectations are often demanding of attention capacity and self-control, and so it is not surprising that many of the efficacious treatments for ADHD have focused on improving academic functioning and classroom behaviors. Children with ADHD are effectively treated with classroom contingency management strategies [ 38 ]. Systematic reviews [ 1 , 2 , 4 , 5 , 39 ] as well as meta-analyses [ 40 , 41 , 42 ] clearly illustrate that behavioral classroom management is an efficacious treatment for ADHD.
As noted above, behavioral classroom management is an efficacious treatment for ADHD. Before discussing evidence for efficacy and effectiveness of behavior classroom management, it is worth noting approaches that do not strongly support positive outcomes. In the United States, children with ADHD are eligible for behavioral classroom management support through Section 504 Accommodation plans administered through the Americans with Disabilities Act or through an Individualized Education Program if the committee on special education determines it is needed. These policies have provided school-based behavioral supports for students with ADHD for over 30 years. However, given that follow-up studies indicate that the long-term educational outcomes for students with ADHD are modest, at best [ 43 , 44 , 45 , 46 ], it is important to emphasize that these accommodation plans or individualized education programs are only useful if they include effective interventions and supports for the child or adolescent with ADHD.
Practically speaking, behavioral classroom management approaches that are effective will include setting clear goals and rules, ensure that the child receives clear feedback on progress toward meeting goals, and that consequences, typically rewards and privileges contingent on meeting behavioral goals and following rules, are provided liberally. It is important to note that positive behavior support strategies are interwoven into the fabric of elementary school classrooms - teachers provide rules and structure for activities, there is praise issued for appropriate behavior, and schools have standard discipline procedures including office referrals or detentions for rule violations. Feedback is provided on a regular, if infrequent basis (i.e., on quarterly report cards). For most children with ADHD this provides a reasonable baseline of behavioral classroom management, but additional strategies and supports are typically needed to make the overall approach to supporting a child with ADHD more efficacious.
Children with ADHD typically need much more frequent behavioral feedback and positive consequences for appropriate behavior in schools. For that reason, a daily report card is among the most efficacious positive behavior supports within a classroom [ 47 , 48 ]. The daily report card has long been used effectively to treat ADHD, monitor outcomes, and open a daily line of communication between teachers and the child’s parent [ 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 ], and it is a procedure aligned with a long tradition of using contingency management with children with disruptive behavior in general educational settings [ 58 ] and in special education settings [ 57 , 59 , 60 ]. In addition to being among the most efficacious classroom interventions, it is also one of the most cost effective [ 61 ].
Recent changes in the ways schools address social, emotional, and behavioral challenges may promote greater effectiveness of the implementation of classroom behavior management strategies. Multi-tiered systems of support (MTSS [ 62 ] in schools conceptualize the behavior of children as being within a continuum, and through regular screening and progress monitoring, provide more intensive intervention, when indicated and for as long as is needed. Currently MTSS efforts in schools are focused on academic achievement targets, and there is less emphasis on MTSS for behavior [ 63 ]. However, the MTSS model of screening and intervention is similar to the single case design approach to intervention that has been long-used within the ADHD treatment literature [ 4 , 5 , 47 ]. In this approach, following the collection of baseline data, behavior classroom management interventions are systematically introduced to evaluate their effectiveness. Educators also benefit from ongoing coaching, support, and monitoring of progress to promote consistent and protracted use of these behavioral interventions [ 64 ].
Supporting this approach to school-based intervention is a recent study that evaluated the effectiveness of different sequences of ADHD treatment [ 65 ]. In this study, using a sequential, multiple assignment randomized trial (SMART [ 66 ]), children were randomly assigned to begin the school year with one of the two evidence-based treatments for ADHD - a low dose of stimulant medication or an initial course of behavior therapy (eight parent training sessions and a daily report card intervention at school). Teachers provided feedback on how the child was functioning in the classroom, and if there was evidence of impaired functioning, the child was then randomly assigned to more treatment – either a greater dose of the treatment at the start of the school year, or a other modality. Thus, children could have a treatment sequence of: (1) medication followed by an increased dose of medication; (2) medication with behavior therapy added; (3) behavior therapy followed by an increased dose of behavior therapy; or (4) behavior therapy followed by medication. Results were interesting as they illustrated the best sequence of treatment for reducing discipline referrals and disruptive behaviors observed in the classroom were those that started with behavior therapy first. Further, the behavior therapy first approaches also cost less to implement across the school year than the treatment sequences that included medication [ 61 ]. Importantly, this study of the effectiveness of treatment sequencing spanned an entire school year, improving upon the research base of efficacy treatments where many studies focused on shorter time periods. While the Pelham study provides a foundation for considering combined and sequenced approaches, far less has been done on the effectiveness of behavioral classroom approaches when conducted within and supported entirely by school-staff over the course of multiple school years.
Overall, there is strong support for behavioral classroom interventions, including the Daily Report Card [ 48 , 50 , 67 ], and it is strongly recommended that this intervention be initiated for children with ADHD experiencing classroom-based impairment. For older children (e.g., middle school, high school), a behavioral contract may be used to initiated contingency management across the multiple classrooms characteristic of this grade level. Educators and parents should ensure that school-based interventions are implemented consistency and continuously, as school-based behavioral challenges are likely to extend across school years and grade levels.
Organization skills training
Related to their difficulties staying on task and following the rules in the classroom setting, children with ADHD have impaired organization, time management, and planning skills that undermine their academic abilities and potential. Homework management and organizational skills have been shown to predict concurrent GPA and later academic outcomes [ 68 , 69 ]. Organizational skills training (OST) interventions utilize behavioral methods to teach skills directly to students with ADHD. The training programs often include behavioral management procedures administered by a counselor, parent, or teacher to reinforce skill use and progress in treatment. Organizational interventions have largely targeted middle school to early high school students with ADHD (ages 10–14 [ 70 ]), with sessions focusing on materials organization, understanding time and time management, and planning larger assignments. Session frequency and length vary widely from about 10, 60-minute family sessions in a clinic [ 71 ] to 40, 2.5-hour student sessions in an after-school setting [ 72 ]. Multicomponent OST packages lead to improvements in organizational skills, planner use, and adolescent impairment [ 73 ].
Embedding OST in schools is key to enhancing the reach of these interventions. Though availability of school personnel to implement OST varies across districts, current work aims to train school counselors to implement OST with students with ADHD [ 74 ]. Langberg and colleagues [ 74 ] found that OST delivered by school staff led to improvements in organization, time management, and planning skills as performance and behavior during homework based on parent-report. Importantly, these results were found despite the school counselors receiving only 2 h of training in the intervention with no ongoing supervision. Purposefully limiting training and post-training investment allows for the examination of treatment effects in the context in which they would likely be provided—i.e., in schools, by school mental health providers with little funding for training and ongoing supervision. Toward the same goal of increasing the sustainability of OST within schools, investigators are developing online tools to assist school staff with OST implementation at low to no cost [ 75 ].
Psychosocial treatments for children with ADHD have primarily been researched in elementary-age youth, and early work in developing organizational skills interventions addressed this gap by upwardly extending treatments to middle school age youth. As the evidence accumulated that such interventions were efficacious among children with ADHD in middle school [ 1 , 2 ], further developmental extension was clearly justified [ 76 ]. adapted their OST program developed for middle schoolers to pilot with high school students with ADHD. Pilot data demonstrated feasibility and indicated that high schoolers may need about 50 sessions to benefit from the OST program. In the full-scale randomized clinical trial [ 77 ], high schoolers attended an average of 40 brief OST sessions while their caregivers attended an average of 4 behavioral parent training sessions. Compared to the control group, beneficial effects of treatment were found on parent-reported academic functioning and organizational skills, and no significant effects on grades, teacher-reported, or self-reported outcomes were found. Results are promising, and much more work is needed to support the academic functioning of older adolescents with ADHD.
Digital therapeutics
Of all the available non-medication treatments, this category is the only one that features protocols patented by the US Patent and Trademark Office (USPTO) and cleared by the U.S. Food and Drug Administration (FDA) for the treatment of ADHD. It is also the most controversial, with competing consensus statements concluding that these types of interventions have proven effective vs. proven ineffective [ 78 ], millions of dollars in fines for false advertising [ 78 ], and a perceived disconnect between benchmarks for effectiveness between the FDA and professional organizations that evaluate psychosocial treatments for children [ 79 ]. Overall, there appears to be evidence for small benefits of cognitive training on reducing inattentive symptoms, and potentially overall ADHD symptoms [ 80 ]. However, we contend that omnibus meta-analytic effect sizes are fundamentally uninterpretable in the context of cognitive training/digital therapeutics because the treatments that fall under this general umbrella feature wide variations in neurocognitive/neurological training targets, conceptual models of neurocognition that define these intended training targets, success/failure to meaningfully engage and improve the intended training target(s), and technologies employed to ‘hit’ the intended target(s). Therefore, what these treatments share are more peripheral features, rather than core mechanistic features necessary to meet meta-analytic assumptions. Even interventions given the same, more specific label (e.g., “working memory training”) vary widely in their approach, conceptual basis, and success/failure at engaging their mechanistic target as shown previously [ 81 ]. It will be important for the field to evaluate each intervention on its own merits because these protocols generally share very little with each other except for the use of a serious games approach [ 82 ] to engaging children in treatment.
Several neurocognitive training protocols have been developed and tested for children with ADHD; we briefly review three of the most prominent: EndeavorRX, CogMed, and Central Executive Training (Cenextra; an intervention developed by one of the co-authors). All three of these approaches are computerized digital therapeutics that include gaming elements and adaptive changes in difficulty. EndeavorRX trains cognitive attention abilities [ 83 ], Cenextra trains the ‘working’ components of working memory [ 84 ] and CogMed is intended to improve attention and working memory abilities [ 85 ], though clinical trial and meta-analytic evidence indicates that CogMed successfully engages short-term memory but not working memory abilities [ 81 , 86 , 87 ].
In terms of efficacy, EndeavorRX showed early promise in pilot/uncontrolled studies given generally favorable feasibility, acceptability, and engagement data [ 83 ]. In addition, EndeavorRX showed potential for reductions in parent-reported ADHD symptoms in proof-of-concept and open-label trials with children with ADHD [ 88 , 89 ]. However, the only controlled trial to date [ 83 ] demonstrated that these potential reductions were likely attributable to placebo effects – that is, Endeavor RX failed to show superior improvements in ADHD behavioral symptoms relative to a control condition (a spelling game). Evans et al. [ 79 ] concluded that “there is no evidence that using this game will result in any benefit in terms of their functioning and presenting problems.” (p. 125).
Cenextra also showed early promise in a head-to-head comparison with behavioral parent training (BPT) indicating favorable feasibility, acceptability, and engagement data. Cenextra was superior to BPT for improving working memory ( d = 1.06) and reducing objectively-assessed hyperactivity ( d = 0.74), and equivalent to BPT for reducing parent-reported ADHD symptoms at post-treatment [ 90 ]. These benefits were largely confirmed in an RCT comparing Cenextra with an active, credible digital therapeutic control called Inhibitory Control Training (ICT; [ 84 ]). Evidence suggesting improved functional outcomes is also emerging, and includes superior improvements relative to both BPT and ICT on masked teacher perceptions of organizational skills, academic success, impulse control, and academic productivity 1–2 months after treatment ended [ 91 , 92 ].
Similar to EndeavorRX and Cenextra, Cogmed showed considerable promise in early trials, and is arguably the most extensively studied neurocognitive training program. Results from meta-analytic reviews and RCTs, however, suggest that CogMed does not improve working memory, but rather improves select components of short-term memory (meta-analytic d = 0.63; [ 81 , 86 , 93 , 94 ]. This is an important limitation for at least two reasons: First, most children with ADHD do not have deficits in short term memory (20–38% impairment rates) despite the majority having impairments in working memory (75–81%; [ 95 , 96 , 97 ]). Second, short-term memory abilities are not significantly associated with ADHD symptoms in most studies [ 81 , 95 ], which suggests limited potential for downstream improvements in ADHD behavioral symptoms. Indeed, conclusions from multiple meta-analytic reviews suggest that benefits on ADHD behavioral symptoms from CogMed are generally limited to unblinded parent ratings [ 81 , 93 ]. Notably, however, a more recent meta-analysis published by the developer of CogMed suggests significant, small benefits for reducing inattention ( d = 0.37; [ 98 ]), though the extent to which this was driven by unblinded parent ratings was unclear.
A key benefit of digital therapeutics – and ‘software as medicine’ in general – is that they have the potential to continually adapt and improve based on real-time patient data. Thus, it is possible that interventions that are not showing the behavioral/functional benefits we had hoped for now could begin to do so in the future. Thus, we highlight some key areas for improvement based on conceptual models and the limited available literature on moderators of cognitive training efficacy for children with ADHD. First, there is a need to maximize dosage . In the context of digital therapeutics, ‘dosage’ refers to the quantity and quality of time spent actively engaging with the training exercises. Most existing protocols have been studied over a relatively limited time frame of 4–10 weeks of training, with a total training time of about 10–12 h across intervention protocols [ 83 , 84 , 99 ]. It is possible that this level of training is insufficient for producing large enough neurocognitive improvements to translate into meaningful – and statistically detectable – gains in downstream behavioral/functional outcomes, suggesting the need for more intensive/longer duration training.
An option closely related to maximizing dosage is increasing the specificity of the neurocognitive training target(s). Although training a variety of neurocognitive functions is appealing at face value, meta-analytic evidence indicates that such protocols produce smaller near-transfer effects than protocols that focus on a single neurocognitive training target [ 81 ]. It is presumed that the reason for this finding is that the more different cognitive ‘muscles’ that we are trying to train, the less time we can spend on any one of those ‘muscles’. Thus, it appears likely that maximizing efficacy will require separate protocols for each neurocognitive function that is impaired in ADHD, combined with a ‘personalized medicine’ approach in which each child’s neurocognitive profile is estimated at pre-treatment, and then a treatment plan is developed to target each of their identified weaknesses. We must leverage basic science to link training targets with behavioral/functional outcomes . Related to dosage and specificity issues is the idea of matching neurocognitive training targets with the specific outcome(s) of interest. Stated bluntly, neurocognitive training is not likely to be helpful if we are training neurocognitive abilities that are not robustly linked with the reason(s) a child presents for treatment. On the other hand, neurocognitive training protocols have great potential if they are able to produce robust improvements in their training target, and if that training target is robustly associated with the observable behaviors/functional outcomes we are trying to improve. A final area that shows promise for improving the efficacy of digital therapeutic interventions is augmentation: Combining them with existing treatments to (potentially) produce synergistic and/or augmentative benefits. This area of inquiry is in its infancy, and currently shows more conceptual promise than actual benefits [ 100 ].
Future directions in improving efficacy and effectiveness
This brief review of psychosocial treatments for ADHD illustrates the robust evidence in support of these interventions. Importantly, there is no panacea or magic bullet for ADHD; the interventions reviewed herein have notable limitations and response to interventions vary. As such, there continues to be efforts at refining existing approaches and developing novel approaches to treating the complex presentation of ADHD. We highlight here what we believe are key future directions, broadly speaking, in improving the effectiveness and efficacy of treatment for ADHD. These fall under two broad areas: future directions in treatments and future directions in service delivery of these treatments.
Future directions in treatment for ADHD
Moderators of treatment effects.
Much of the intervention literature has focused on static factors or social addresses (terms that describe rather than explain; e.g., marital status, child age;) as factors, largely because these are measures of convenience. Efforts toward using dynamic factors have shed light on what works for whom and can further refine an intervention to increase potency. As an example, in BPT, parent-level variables (e.g., parenting stress [ 101 ]) have been shown to moderate BPT engagement and outcomes, suggesting that future refinements to BPT that more directly address parental stress may increase the potency of BPT. Such efforts should be employed across all psychosocial interventions for ADHD. Importantly, as we have discussed elsewhere [ 8 , 102 ], efforts should go beyond variable-centered approaches (e.g., child age, parent stress) toward holistic, person- and/or family-centered approaches (the clustering of variables that more fully represent a child/parent/family). As an example, Dale et al. [ 103 ] employed a person-centered approach to create subgroups of families based on the intersection of multiple parent, child, and family factors to understand response to BPT for families of preschool children with ADHD. Three distinct family profiles emerged, with data suggesting differential response for families with high stress, elevated parental anxiety, and elevated parental depression. These typological approaches better reflect reality- people are more accurately reflected as a complex intersection of variables rather than just any one variable- and taking this approach may better result in a nuanced understanding of response to treatment and further inform treatment for types of people and families.
ADHD is complex and presentations vary. It is not uncommon for children and adolescents with ADHD to also have significant difficulties outside of core symptoms of ADHD (e.g., emotion dysregulation, sleep disturbances) that may moderate treatment response. As an example, ADHD is frequently associated with emotional regulation challenges, with studies suggesting that the vast majority of children with ADHD (i.e., 75%) have some symptoms of emotion dysregulation, with 25% having severe emotion dysregulation [ 104 ]. In fact, children with ADHD and severe emotion dysregulation are more likely to have complex presentations, cross-situational impairments and severe psychopathology [ 105 ]. Interestingly, there are few rigorous randomized controlled trials evaluating the effects of psychosocial interventions for emotion dysregulation in children with ADHD [ 106 ]. These and other moderators may best be evaluated through novel approaches such as individual participant data meta-analysis [ 107 ]. Addressing the needs of youth with ADHD and their families will require going beyond addressing core symptoms of ADHD. In fact, we have long argued that these types of functional impairments (e.g., academic, social functioning) should be the targets for ADHD treatment rather than ADHD symptoms [ 8 ].
Novel intervention targets
The presentation of ADHD at key developmental periods/tasks may pose significant challenges for affected youth and their families- necessitating novel targets of intervention. An example of this is the transition to learning to drive. Adolescents are the riskiest drivers on the roadway, overall; if an adolescent has ADHD they are significantly more at risk for negative driving outcomes including accidents, accidents that cause injury, and fatalities [ 108 , 109 ]. The period of time when individuals with ADHD are learning to drive may therefore be a critical, and also opportune time to initiate intervention. A recent RCT with adolescents with ADHD [ 110 ], evaluated a specially designed computerized simulated-driving program with feedback and found reduced problematic driving as compared with a control program. During real-world driving in the year after training, the rate of collisions and near-collisions was lower in the intervention group. These efforts highlight the potential of psychosocial interventions for addressing impairments inherent with developmental transitions for youth with ADHD. Related work suggests that intervening with adolescents at the transition to middle school and high school with intensive summer “bridge” programs may be a useful approach with high levels of engagement [ 111 ]. Future work should focus on embedding treatment efforts into other developmental tasks/transitions/tasks (e.g., start of preschool or initiation of employment).
Future directions in service delivery
ADHD is now very clearly understood to persist throughout development and into adulthood and there has rightfully been a shift toward a chronic care model [ 7 ]. Given this, attention must be given to developing integrated, consistently available and longitudinal approaches embedded in routine service systems such that children, adolescents (and even adults) with ADHD and their families can receive appropriate care. Unfortunately, availability and access to evidence-based interventions are limited. Recent studies suggest that only 31% of families of children with ADHD receive BPT [ 21 ] and just 32% receive behavioral classroom management [ 112 ]. Given this, we highlight herein issues related to increasing availability and access to evidence-based psychosocial treatment for ADHD- important goals to help close the science-to-service-gap in ADHD. More specifically, we briefly highlight efforts on (1) leveraging the existing workforce, and (2) using technology to deliver evidence-based psychosocial treatments.
Leveraging existing workforces
In light of mental health workforce shortages ( https://data.hrsa.gov/topics/health-workforce/workforce-projections ) new models of care will need to utilize and expand existing, but underdeveloped, non-professional and paraprofessional workforces [ 31 , 32 ]. One example of a sustainable, scalable model of care is the Family Peer Advocate (FPA) ADHD Model [ 25 ]. FPAs are part of a national family support model of current and former parent/caregivers of children with identified mental health needs who provide a range of services, including parenting skills training, emotional support, education about mental health services, and direct advocacy [ 30 ]. FPA-services are flexibly delivered in a variety of parent-identified settings (e.g., parent’s homes, community settings) and often connect and engage parents with key service settings/providers (e.g., schools, primary care, mental health clinics), reducing the systemic barriers associated with traditional service delivery models. Moreover, FPAs have many shared experiences with the families they serve including personal experience with providing care and navigating the service system for children with mental health challenges, often within the same community as those they serve. As a result, FPA care is associated with high acceptability ratings and increased engagement [ 113 ]. This FPA Model appears to be especially effective in reaching ethnically diverse families from socioeconomically disadvantaged backgrounds [ 30 , 113 ]. Emerging data suggest that FPAs can reliably and effectively deliver BPT for youth with ADHD [ 25 ], suggesting that this and other workforce (e.g., ADHD Coaches) should be leveraged in order to increase availability and access to evidence-based psychosocial interventions for ADHD.
The idea of leveraging the existing workforce also applies to school settings. The MTSS intervention framework, which embeds intervention in schools into universal, targeted, and indicated approaches is an example of a potential means of re-allocating professional time and expertise. Rather than waiting for school psychologists and special educators to get involved only when the child is considered for special education, a MTSS approach might utilize the expertise of these professionals to consult with the general education teacher on how to implement positive behavior supports for a child with ADHD. In this way, intervention is implemented quicker, in the setting where the initial impairment is identified, by existing school professionals [ 56 , 114 ].
Use of technology
Technology-based approaches to delivering evidence-based interventions have the potential to revolutionize mental health service access and delivery across multiple mental health disorders [ 115 ]. Online self-directed BPT approaches are potentially more feasible, affordable, and acceptable, can have significant reach to include traditionally underserved populations, and are readily scalable and sustainable [ 116 , 117 ]. Over 13 studies have recently been conducted demonstrating that online BPT can improve child behavioral outcomes. Importantly, a recently published trial compared Triple P Online (TPO; an evidence-based, commercially available, self-directed online BPT) to a face-to-face (F2F) therapist-delivered Triple P for preschool children with disruptive behavior problems [ 118 ]. This large randomized controlled trial found that TPO was non-inferior to F2F Triple P on observed and parent-reported child behavior, with clinically meaningful effect sizes. This study, combined with several other studies [ 27 , 119 , 120 ] demonstrate the effectiveness of online BPT in general and specifically for ADHD. Technology is increasingly being utilized in practice settings (e.g., ADHD Care Assistant in primary care [ 121 ]; Online Daily Report Card in schools [ 122 ]) to increase access to evidence-based psychosocial interventions. Concerted efforts and rigorous empirical investigation will be necessary to further determine the effectiveness of these approaches. Importantly, while there is high potential for such technology-delivered approaches, engagement to these formats will remain important to address [ 123 ].
Conclusions
ADHD is a prevalent, pervasive, chronic and impairing disorder that necessitates early, integrated, continuous interventions over a child’s development. Fortunately, several psychosocial interventions are available that address key functional impairments in children and adolescents with ADHD. Given the complex presentation of ADHD, novel approaches to address both underlying pathophysiological mechanisms associated with ADHD (e.g., working memory) as well as domains closely impacted in those with ADHD (e.g., emotion regulation) and key developmental tasks (e.g., driving) are emerging areas in ADHD intervention science. Efforts to improve the efficacy of psychosocial interventions remain important as the acute benefits of these interventions do not result in normalized functioning for many youth and there remains an under-appreciation for whom these interventions are most impactful. Likely most pressing is the translation of the intervention science to improve outcomes for the millions of youth affected by ADHD, the science-to-service gap is prominent; many children who can benefit from evidence-based psychosocial interventions do not receive them. Improving access and availability of evidence-based psychosocial interventions remains critical to ensure that the significant efforts made over decades in developing and evaluating interventions for ADHD result in population-level benefits for youth with ADHD.
Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2014;43:527–51.
Article PubMed Google Scholar
Evans SW, Owens JS, Wymbs BT, Ray AR. Evidence-based psychosocial treatments for children and adolescents with attention deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2018;47:157–98.
Pelham WE Jr, Fabiano GA. Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2008;37:184–214.
Pelham WE Jr, Wheeler T, Chronis A. Empirically supported psychosocial treatments for attention deficit hyperactivity disorder. J Clin Child Adolesc Psychol. 1998;27:190–205.
Article Google Scholar
Barbaresi WJ, Campbell L, Diekroger EA, Froehlich TE, Liu YH, O’Malley, et al. Society for Developmental and Behavioral Pediatrics clinical practice guideline for the assessment and treatment of children and adolescents with complex attention-deficit/hyperactivity disorder. J Dev Behav Pediatr. 2020;41:S35–S57.
American Academy of Child and Adolescent Psychiatry. Practice parameters for assessment and treatment of children and adolescents with Attention-Deficit/Hyperactivity Disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:894–921.
DuPaul GJ, Evans SW, Mautone JA, Owens JS, Power TJ. Future directions for psychosocial interventions for children and adolescents with ADHD. J Clin Child Adolesc Psychol. 2020;49:134–45.
Chacko A, Alan C, Uderman J, Cornwell M, Anderson L, Chimiklis A. Ch 10. In: Barkley R, editor. Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment, 4th edn. New York: Guilford Press; 2015.
Chacko A, Wymbs BT, Arnold FW, Pelham WE, Swanger-Gagne M, Girio EL, et al. Enhancing traditional behavioral parent training for single-mothers of children with ADHD. J Clin Child Adolesc Psychol. 2009;38:206–18.
Chacko A, Wymbs BT, Chimiklis A, Wymbs FA, Pelham WE. Evaluating a comprehensive strategy to improve engagement to group-based behavioral parent training for high-risk families of children with ADHD. J Abnorm Child Psychol. 2012;40:1351–62.
Gerdes AC, Kapke TL, Grace M, Castro A. Feasibility, acceptability, and preliminary outcomes of a culturally-adapted evidence-based treatment for Latino youth with ADHD. J Atten Disord. 2021;25:432–47.
Fabiano GA, Pelham WE, Cunningham CE, Yu J, Gangloff B, Buck M, et al. A waitlist-controlled trial of behavioral parent training for fathers of children with ADHD. J Clin Child Adolesc Psychol. 2012;41:337–45.
Article PubMed PubMed Central Google Scholar
Barkley RA, Benton CM. Your defiant child: eight steps to better behavior. Chicago: Guilford Press; 2013.
Leijten P, Melendez-Torres GJ, Knerr W, Gardner F. Transported versus homegrown parenting interventions for reducing disruptive child behavior: a multilevel meta-regression study. J Am Acad Child Adolesc Psychiatry. 2016;55:610–7.
Rajwan E, Chacko A, Wymbs BT, Wymbs FA. Evaluating clinically significant change in parent and child functioning: Comparison of traditional and enhanced behavioral parent training. J Abnor Chil Psychol. 2014;42:1407–12.
Marquet-Doléac J, Biotteau M, Chaix Y. Behavioral parent training for school-aged children with ADHD: a systematic review of randomized control trials. J Atten Disord. 2023;28:377–93.
Doffer DPA, Dekkers T, Hornstra R, van der Oord S, Luman M, Leijten P, et al. Sustained improvements by behavioural parent training for children with attention-deficit/hyperactivity disorder: a meta-analysis into longer-term child and parental outcomes. JCCP Adv. 2023;3:e12196.
Fabiano GA, Schatz NK, Aloe AM, Pelham WE Jr, Smyth AC, Zhao X, et al. Comprehensive meta-analysis of attention-deficit/hyperactivity disorder psychosocial treatments investigated within between group studies. Rev Educ Res. 2021;91:718–60.
Cohen J. Things I have learned (so far). In: Annual Convention of the American Psychological Association, 98th, 1990, Boston, MA, USA; Presented at the aforementioned conference. American Psychological Association; 1992.
Wolraich ML, Hagan JF, Allan C, Chan E, Davison D, Earls M, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2019;144:e20192528.
Danielson ML, Visser SN, Chronis-Tuscano A, DuPaul GJ. A national description of treatment among U.S. children and adolescents with ADHD. J Pediatr. 2018;192:240–6.
Ortiz C, Vidair HB, Acri M, Chacko A, Kobak K. Pilot study of an online parent-training course for disruptive behavior with live remote coaching for practitioners. Prof Psychol Res Pract. 2020;51:125–33.
Chacko A, Jensen S, Lowry LS, Cornwell M, Chimiklis A, Chan E, et al. Engagement in behavioral parent training: review of the literature and implications for practice. Clin Child Fam Psychol Rev. 2016;19:204–15.
Sanchez AL, Jent J, Aggarwal NK, Chavira D, Coxe S, Garcia D, et al. Person-centered cultural assessment can improve child mental health service engagement and outcomes. J Clin Child Adolesc Psychol. 2022;51:1–22.
Chacko A, Hopkins K, Acri M, Mendelsohn A, Dreyer B. Expanding ADHD service provision in urban socioeconomically disadvantaged communities: a pilot study. Clin Pract Pediatr Psychol. 2020;8:189–94.
Google Scholar
Chacko A, Isham A, Cleek A, Mckay M. Using mobile health technology to improve homework implementation in evidence-based parenting intervention for disruptive behavior disorders in youth. Pilot Feasibility Stud. 2016;2:1–11.
DuPaul GJ, Kern L, Belk G, Custer B, Daffner M, Hatfield A, et al. Face-to-face versus online behavioral parent training for young children at risk for ADHD: treatment engagement and outcomes. J Clin Child Adolesc Psychol. 2018;47:S369–S383.
Myers K, Vander Stoep A, Zhou C, McCarty CA, Katon W. Effectiveness of a telehealth service delivery model for treating attention-deficit/hyperactivity disorder: a community-based randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2015;54:263–74.
Xie Y, Dixon JF, Yee OM, Zhang J, Chen YA, DeAngelo S, et al. A study on the effectiveness of videoconferencing on teaching parent training skills to parents of children with ADHD. Telemed J E Health. 2013;19:192–9.
Article CAS PubMed Google Scholar
Acri M, Hooley CD, Richardson N, Moaba LB. Peer models in mental health for caregivers and families. Community Ment Health J. 2017;53:241–9.
Chacko A, Scavenius C. Bending the curve: Community based behavioral parent training to address ADHD symptoms in the voluntary sector in Denmark. J Abnorm Child Psychol. 2018;46:505–17.
Chacko A, Gopalan G, Franco L, Dean-Assael K, Jackson J, Marcus S, et al. Multiple-Family Group service delivery model for the children with disruptive behavior disorders. J Emot Behav Disord. 2015;23:67–77.
Van der Oord S, Tripp G. How to improve behavioral parent and teacher training for children with ADHD: Integrating empirical research on learning and motivation into treatment. Clin Child Fam Psychol Rev. 2020;23:577–604.
Furukawa E, Alsop B, Sowerby P, Jensen S, Tripp G. Evidence for increased behavioral control by punishment in children with attention-deficit hyperactivity disorder. J Child Psychol Psychiatry. 2017;3:248–57.
Furukawa E, Alsop B, Shimabukuro S, Tripp G. Is increased sensitivity to punishment a common characteristic of attention deficit/hyperactivity disorder? An experimental study of response allocation in Japanese children. Atten Deficit Hyperact Disord. 2019;11:433–43.
Sonuga-Barke EJ, Thompson M, Abikoff H, Klein R, Brotman LM. Nonpharmacological interventions for preschoolers with ADHD: The case for specialized parent training. Infants Young Child. 2006;19:142–53.
Abikoff HB, Thompson M, Laver‐Bradbury C, Long N, Forehand RL, Miller Brotman L, et al. Parent training for preschool ADHD: a randomized controlled trial of specialized and generic programs. J Child Psychol Psychiatry. 2015;56:618–31.
DuPaul GJ. Attention deficit-hyperactivity disorder: classroom intervention strategies. Sch Psychol Int. 1991;12:85–94.
Harrison JR, Soares DA, Rudzinski S, Johnson R. Attention deficit hyperactivity disorders and classroom-based interventions: Evidence-based status, effectiveness, and moderators of effects in single-case design research. Rev Educ Res. 2019;89:569–611.
DuPaul GJ, Eckert TL. The effects of school-based interventions for attention deficit/hyperactivity disorder: a meta-analysis. Sch Psych Rev. 1997;26:5–27.
DuPaul GJ, Eckert TL, Vilardo B. The effects of school-based interventions for attention deficit hyperactivity disorder: A meta-analysis 1996–2010. Sch Psych Rev. 2012;41:387–412.
Fabiano GA, Pelham WE Jr, Coles EK, Gnagy EM, Chronis-Tuscano A, O’Connor BC. A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clin Psychol Rev. 2009;29:129–40.
Arnold LE, Hodgkins P, Kahle J, Madhoo M, Kewley G. Long-term outcomes of ADHD: academic achievement and performance. J Atten Disord. 2020;24:73–85.
Kent KM, Pelham WE, Molina BS, Sibley MH, Waschbusch DA, Yu J, et al. The academic experience of male high school students with ADHD. J Abnorm Child Psychol. 2011;39:451–62.
Kuriyan AB, Pelham WE, Molina BS, Waschbusch DA, Gnagy EM, Sibley MH, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41:27–41.
Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry 2009. 2009;48:484–500.
Pyle K, Fabiano GA. A meta-analysis of single-subject design studies utilizing the daily report card intervention for students with ADHD. Excep Child. 2017;83:378–95.
Volpe R, Fabiano, GA. Daily behavior report cards: an evidence-based system of assessment and intervention. New York, NY: The Guilford Press; 2013.
Kelley ML. School-home notes: promoting children’s classroom success. New York: The Guilford Press; 1990.
O’Leary KD, Pelham WE, Rosenbaum A, Price GH. Behavioral treatment of hyperkinetic children: an experimental evaluation of its usefulness. Clin Pediatr. 1976;15:510–5.
Owens JS, Holdaway AS, Zoromski AK, Evans SW, Himawan LK, Girio-Herrera E, et al. Incremental benefits of a daily report card intervention over time for youth with disruptive behavior. Behav Ther. 2012;43:848–61.
Pelham WE, Fabiano GA, Massetti GM. Evidence-based assessment for attention-deficit/hyperactivity disorder in children and adolescents. J Clin Child Adolesc Psychol. 2005;34:449–76.
Pelham WE, Gnagy EM, Burrows-Maclean L, Williams A, Fabiano GA, Morrissey SM, et al. Once-a-day Concerta™ methylphenidate versus t.i.d. methylphenidate in laboratory and natural settings. Pediatrics. 2001;10:e105.
Pelham WE, Hoza B, Pillow DR, Gnagy EM, Kipp HL, Greiner AR, et al. Effects of methylphenidate and expectancy on children with ADHD: behavior, academic performance, and attributions in a summer treatment program and regular classrooms. J Consult Clin Psychol. 2002;70:320–35.
Pfiffner LJ, Mikami AY, Huang-Pollock C, Easterlin B, Zalecki C, McBurnett K. A randomized, controlled trial of integrated home-school treatment for ADHD, Primarily inattentive type. J Am Acad Child Adolesc Psychiatry. 2007;46:1040–51.
Pfiffner LJ, Villodas M, Kaiser N, Rooney M, McBurnett K. Educational outcomes of a collaborative school-home behavioral intervention for ADHD. Sch Psychol Q. 2013;28:25–36.
Vannest KJ, Davis JL, Davis CR, Mason BA, Burke MD. Effective intervention for behavior with a daily behavior report card: a meta-analysis. Sch Psych Rev. 2010;39:654–72.
Hops H, Walker HM. CLASS: contingencies for learning and academic and social skills. Seattle WA: Educational Achievement Systems; 1988.
Reid R, Maag JW, Vasa SF, Wright G. Who are the children with attention deficit-hyperactivity disorder? A school-based survey. J Spec Educ. 1994;28:117–37.
Schnoes C, Reid R, Wagner M, Marder C. ADHD among students receiving special education services: a national survey. Excep Child. 2006;72:483–96.
Page TF, Pelham WE III, Fabiano GA, Greiner AR, Gnagy EM, et al. Comparative cost analysis of sequential, adaptive, behavioral, pharmacological, and combined treatments for childhood ADHD. J Clin Child Adolesc Psychol. 2016;45:416–27.
Burns MK, Jimerson SR, VanDerHeyden AM, Deno, SL. Toward a unified response-to-intervention model: Multi-tiered systems of support. In: Handbook of response to intervention: The science and practice of multi-tiered systems of support. Boston, MA: Springer US; 2015. p. 719–32.
Briesch AM, Chafouleas SM, Nissen K, Long S. A review of state-level procedural guidance for implementing multitiered systems of support for behavior (MTSS-B). J Posit Behav Inter. 2020;23:131–44.
Owens JS, McLennan JD, Hustus CL, Haines-Saah R, Mitchell S, Mixon CS, et al. Leveraging technology to facilitate teachers’ use of a targeted classroom intervention: Evaluation of the Daily Report Card. Online (DRC. O) System. Sch Ment Health. 2019;11:665–77.
Pelham WE, Fabiano GA, Waxmonsky JG, Greiner AR, Gnagy EM, Pelham WE III, et al. Treatment sequencing for childhood ADHD: A multiple-randomization study of adaptive medication and behavioral interventions. J Clin Child Adolesc Psychol. 2016;45:396–415.
Lei H, Nahum-Shani I, Lynch K, Oslin D, Murphy SA. A “SMART” design for building individualized treatment sequences. Annu Rev Clin Psychol. 2012;8:21–48.
Owens JS, Hustus CL, Evans SW. The daily report card intervention: Summary of the science and factors affecting implementation. In: Handbook of research on emotional and behavioral disorders. Routledge; 2020. p. 371–85.
Langberg JM, Epstein JN, Girio-Herrera E, Becker SP, Vaughn AJ, Altaye M. Materials organization, planning, and homework completion in middle-school students with ADHD: impact on academic performance. Sch Ment Health. 2011;3:93–101.
Langberg JM, Molina BSG, Arnold LE, Epstein JN, Altaye M, Hinshaw SP, et al. Patterns and predictors of adolescent academic achievement and performance in a sample of children with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2011;40:519–31.
Bikic A, Reichow B, McCauley SA, Ibrahim K, Sukhodolsky DG. Meta-analysis of organizational skills interventions for children and adolescents with Attention-Deficit/Hyperactivity Disorder. Clin Psychol Rev. 2017;52:108–23.
Sibley MH, Graziano PA, Kuriyan AB, Coxe S, Pelham WE, Rodriguez L, et al. Parent–teen behavior therapy+ motivational interviewing for adolescents with ADHD. J Consult Clin Psychol. 2016;84:699.
Evans SW, Schultz BK, DeMars CE, Davis H. Effectiveness of the challenging horizons after-school program for young adolescents with ADHD. Behav Ther. 2011;42:462–74.
Chan E, Fogler JM, Hammerness P. Treatment of attention-deficit/hyperactivity disorder in adolescents: a systematic review. JAMA. 2016;315:1997–2008.
Langberg JM, Dvorsky MR, Molitor SJ, Bourchtein E, Eddy LD, Smith ZR, et al. Overcoming the research-to-practice gap: a randomized trial with two brief homework and organization interventions for students with ADHD as implemented by school mental health providers. J Consult Clin Psychol. 2018;86:39.
Pfiffner LJ, Dvorsky MR, Friedman LM, Haack LM, Chung S, Charalel JM, et al. Development of a web-based training platform for school clinicians in evidence-based practices for ADHD. Sch Ment Health. 2023;15:49–66.
Evans SW, Schultz BK, DeMars CE. High school–based treatment for adolescents with attention-deficit/hyperactivity disorder: results from a pilot study examining outcomes and dosage. Sch Psych Rev. 2104;43:185–202.
DuPaul GJ, Evans SW, Owens JS, Cleminshaw CL, Kipperman K, Fu Q, et al. School-based intervention for adolescents with attention-deficit/hyperactivity disorder: effects on academic functioning. J Sch Psychol. 2021;87:48–63.
Simons DJ, Boot WR, Charness N, Gathercole SE, Chabris CF, Hambrick DZ, et al. Do “brain-training” programs work? Psychol Sci. 2016;17:103–86.
Evans SW, Beauchaine TP, Chronis-Tuscano A, Becker SP, Chacko A, Gallagher R, et al. The efficacy of cognitive videogame training for ADHD and What FDA clearance means for clinicians. Evid Based Pract Child Adolesc Ment Health. 2021;6:116–30.
Westwood SJ, Parlatini V, Rubia K, Cortese S, Sonuga-Barke EJ. Computerized cognitive training in attention-deficit/hyperactivity disorder (ADHD): a meta-analysis of randomized controlled trials with blinded and objective outcomes. Mol Psychiatry. 2023;28:1402–14.
Rapport MD, Orban SA, Kofler MJ, Friedman LM. Do programs designed to train working memory, other executive functions, and attention benefit children with ADHD? A meta-analytic review of cognitive, academic, and behavioral outcomes. Clin Psychol Rev. 2013;33:1237–52.
Cannon-Bowers J, Bowers C, editors. Serious game design and development: technologies for training and learning. New York: IGI Global; 2010.
Kollins SH, DeLoss DJ, Cañadas E, Lutz J, Findling RL, Keefe RS, et al. A novel digital intervention for actively reducing severity of paediatric ADHD (STARS-ADHD): a randomised controlled trial. Lancet Digit Health. 2020;2:e168–e178.
Kofler MJ, Wells EL, Singh LJ, Soto EF, Irwin LN, Groves NB, et al. A randomized controlled trial of central executive training (CET) versus inhibitory control training (ICT) for ADHD. J Consult Clin Psychol. 2020;88:738–56.
Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlström K, et al. Computerized training of working memory in children with ADHD-a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry. 2005;44:177–86.
Roberts G, Quach J, Spencer-Smith M, Anderson PJ, Gathercole S, Gold L, et al. Academic outcomes 2 years after working memory training for children with low working memory: a randomized clinical trial. JAMA Pediatr. 2016;170:e154568.
Chacko A, Bedard AC, Marks DJ, Feirsen N, Uderman JZ, Chimiklis A, et al. A randomized clinical trial of Cogmed working memory training in school‐age children with ADHD: A replication in a diverse sample using a control condition. J Child Psychol Psychiatry. 2014;55:247–55.
Davis NO, Bower J, Kollins SH. Proof-of-concept study of an at-home, engaging, digital intervention for pediatric ADHD. PLoS ONE. 2018;13:e0189749.
Kollins SH, Childress A, Heusser AC, Lutz J. Effectiveness of a digital therapeutic as adjunct to treatment with medication in pediatric ADHD. NPJ Digit Med. 2021;4:1–8.
Kofler MJ, Sarver DE, Austin KE, Schaefer HS, Holland E, Aduen PA, et al. Can working memory training work for ADHD? Development of central executive training and comparison with behavioral parent training. J Consult Clin Psychol. 2018;86:964.
Singh LJ, Gaye F, Cole AM, Chan ES, Kofler MJ. Central executive training for ADHD: effects on academic achievement, productivity, and success in the classroom. Neuropsychol. 2022;36:330–45.
Chan ESM, Gaye F, Cole AM, Singh LJ, Kofler MJ. Central executive training for ADHD: impact on organizational skills at home and school. A randomized controlled trial. Neuropsychol.
Chacko A, Feirsen N, Bedard AC, Marks D, Uderman JZ, Chimiklis A. Cogmed working memory training for youth with ADHD: a closer examination of efficacy utilizing evidence-based criteria. J Clin Child Adolesc Psychol. 2013;42:769–83.
Sala G, Gobet F. Working memory training in typically developing children: a meta-analysis of the available evidence. Dev Psychol. 2017;53:671–85.
Kofler MJ, Singh LJ, Soto EF, Chan ESM, Miller CE, Harmon SL, et al. Working memory and short-term memory deficits in ADHD: A bifactor modeling approach. Neuropsychol. 2020;34:686–98.
Fosco WD, Kofler MJ, Groves NB, Chan ESB, Raiker JS. Which ‘working’ components of working memory aren’t working in youth with ADHD? J Abnorm Child Psychol. 2020;48:647–60.
Karalunas S, Gustafsson H, Dieckmann N, Tipsord J, Mitchell SH, Nigg J. Heterogeneity in development of aspects of working memory predicts longitudinal attention deficit hyperactivity disorder symptom change. J Abnorm Child Psychol. 2017;126:774–92.
Spencer-Smith M, Klingberg T. Correction: benefits of a working memory training program for inattention in daily life: a systematic review and meta-analysis. PLoS ONE. 2016;11:e0167373.
Klingberg T, Forssberg H, Westerberg H. Training of working memory in children with ADHD. J Clin Exp Neuropsychol. 2002;24:781–91.
Chacko A, Bedard AC, Marks D, Gopalan G, Feirsen N, Uderman J, et al. Sequenced neurocognitive and behavioral parent training for the treatment of ADHD in school-age children. Child Neuro. 2018;24:427–50.
Article CAS Google Scholar
Chacko A, Feirsen N, Rajwan E, Wymbs BT, Wymbs FA. Distinguishing never-attenders, dropouts, and completers to behavioral parent training: The importance of parental cognitions. J Child Fam Stud. 2017;26:950–60.
Vardanian MM, Ramakrishnan A, Peralta S, Siddiqui Y, Shah S, Clark-Whitney E, et al. Clinically significant and reliable change: comparing an evidence-based intervention to usual care. J Child Fam Stud. 2020;29:921–33.
Dale C, Parent J, Forehand R, DiMarzio K, Sonuga-Barke E, Long N, et al. Behavioral parent training for preschool ADHD: family-centered profiles predict changes in parenting and child outcomes. J Clin Child Adolesc Psychol. 2021;51:726–39.
Sobanski E, Banaschewski T, Asherson P, Buitelaar J, Chen W, Franke B, et al. Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): clinical correlates and familial prevalence. J Child Psychol Psychiatry. 2010;51:915–23.
Qian Y, Chang W, He X, Yang L, Liu L, Ma Q, et al. Emotional dysregulation of ADHD in childhood predicts poor early-adulthood outcomes: a prospective follow up study. Res Dev Disabil. 2016;59:428–36.
Vacher C, Goujon A, Romo L, Purper-Ouakil D. Efficacy of psychosocial interventions for children with ADHD and emotion dysregulation: a systematic review. Psychiatry Res. 2020;291:113–51.
Groenman AP, Hornstra R, Hoekstra PJ, Steenhuis L, Aghebati A, Boyer BE, et al. An individual participant data meta-analysis: behavioral treatments for children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2022;61:144–58.
Aduen PA, Cox DJ, Fabiano GA, Garner AA, Kofler MJ. Expert recommendations for improving driving safety for teens and adult drivers with ADHD. ADHD Rep. 2019;27:8.
Aduen PA, Kofler MJ, Sarver DE, Wells EL, Soto EF, Cox DJ. ADHD, depression, and motor vehicle crashes: A prospective cohort study of continuously-monitored, real-world driving. J Psychiatr Res. 2018;101:42–49.
Epstein JN, Garner AA, Kiefer AW, Peugh J, Tamm L, MacPherson RP, et al. Trial of training to reduce driver inattention in teens with ADHD. N Engl J Med. 2022;387:2056–66.
Sibley MH, Coxe SJ, Campez M, Morley C, Olson S, Hidalgo-Gato N, et al. High versus low intensity summer treatment for ADHD delivered at secondary school transitions. J Clin Child Adolesc Psychol. 2018;47:248–65.
DuPaul GJ, Chronis-Tuscano A, Danielson ML, Visser SN. Predictors of receipt of school services in a national sample of youth with attention-deficit/hyperactivity disorder. J Atten Disord. 2019;23:1303–19.
Hoagwood KE, Cavaleri MA, Serene Olin S, Burns BJ, Slaton E, et al. Family support in children’s mental health: A review and synthesis. Clin Child Fam Psychol Rev. 2010;13:1–45.
Fabiano GA, Pyle K. Best practices in school mental health for attention-deficit/hyperactivity disorder: A framework for intervention. Sch Ment Health. 2019;11:72–91.
Nieuwboer CC, Fukkink RG, Hermanns JM. Online programs as tools to improve parenting: a meta-analytic review. Child Youth Ser Rev. 2013;35:1823–9.
Tan-MacNeill KM, Smith IM, Johnson SA, Chorney J, Corkum P. A systematic review of online parent-implemented interventions for children with neurodevelopmental disorders. Child Health Care. 2021;50:239–77.
Thongseiratch T, Leijten P, Melendez-Torres GJ. Online parent programs for children’s behavioral problems: a meta-analytic review. Eur Child Adolesc Psychiatry. 2020;29:1555–68.
Prinz RJ, Metzler CW, Sanders MR, Rusby JC, Cai C. Online‐delivered parenting intervention for young children with disruptive behavior problems: a noninferiority trial focused on child and parent outcomes. J Child Psychol Psychiatry. 2022;63:199–209.
Baker S, Sanders MR, Turner KM, Morawska A. A randomized controlled trial evaluating a low-intensity interactive online parenting intervention, Triple P Online Brief, with parents of children with early onset conduct problems. Behav Res Ther. 2017;91:78–90.
Franke N, Keown LJ, Sanders MR. An RCT of an online parenting program for parents of preschool-aged children with ADHD symptoms. J Atten Disord. 2020;24:1716–26.
Power TJ, Michel J, Mayne S, Miller J, Blum NJ, Grundmeier RW, et al. Coordinating systems of care using health information technology: development of the ADHD care assistant. Adv Sch Ment Health Promot. 2016;9:201–18.
Mixon CS, Owens JS, Hustus C, Serrano VJ, Holdaway AS. Evaluating the impact of online professional development on teachers’ use of a targeted behavioral classroom intervention. Sch Ment Health. 2019;11:115–28.
Breider S, de Bildt A, Nauta MH, Hoekstra PJ, van den Hoofdakker BJ. Self-directed or therapist-led parent training for children with attention deficit hyperactivity disorder? A randomized controlled non-inferiority pilot trial. Internet Interv. 2019;18:100262.
Coghill D, Banaschewski T, Cortese S, Asherson P, Brandeis D, Buitelaar J, et al. The management of ADHD in children and adolescents: bringing evidence to the clinic: perspective from the European ADHD Guidelines Group (EAGG). Eur Child Adolesc Psychiatry. 2021;32:1337–61.
Download references
Author information
Authors and affiliations.
New York University, New York, NY, USA
Anil Chacko
Florida International University, Miami, FL, USA
Brittany M. Merrill & Gregory A. Fabiano
Florida State University, Tallahassee, FL, 32306, USA
Michael J. Kofler
You can also search for this author in PubMed Google Scholar
Contributions
AC, BM, MJK and GAF were involved in the development, writing, review, revisions and final approval of the manuscript.
Corresponding author
Correspondence to Anil Chacko .
Ethics declarations
Competing interests.
MJK holds a patent for neurocognitive interventions that target central executive working memory and inhibitory control and that were recently licensed to Sky Therapeutics, a company for which MJK provides consulting and holds equity.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Chacko, A., Merrill, B.M., Kofler, M.J. et al. Improving the efficacy and effectiveness of evidence-based psychosocial interventions for attention-deficit/hyperactivity disorder (ADHD) in children and adolescents. Transl Psychiatry 14 , 244 (2024). https://doi.org/10.1038/s41398-024-02890-3
Download citation
Received : 16 January 2023
Revised : 14 February 2024
Accepted : 22 March 2024
Published : 08 June 2024
DOI : https://doi.org/10.1038/s41398-024-02890-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES