Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies

Our 2023/24 business plan
August 2023
Foreword from our chair
We are creating a new organisation following the legal merger of NHS England with NHS Digital on 1 February 2023, and Health Education England on 1 April 2023. This new NHS England will be smaller, more efficient and joined up, and speak with one voice to systems.
NHS England operates under a mandate from government and has a duty to seek to achieve the objectives set out within it, which are under four headings:
- Cut NHS waiting lists and recover performance.
- Support the workforce through training, retention and modernising the way staff work.
- Deliver recovery through the use of data and technology.
- Continue work to deliver the NHS Long Term Plan to transform services and improve outcomes.
This business plan incorporates the actions we will take to meet the 2023 mandate objectives and deliver on our purpose to lead the NHS in England to deliver high-quality services for all. The NHS England Board will oversee its implementation to ensure we make real progress for the patients and populations we serve.
The NHS resource budget for 2023/24 is £168.8 billion and the Government expects NHS England to ensure that overall financial balance is delivered for the NHS each and every year. We will continue to support the NHS in making the most effective use of this public money.
This is an ambitious programme made possible through the extraordinary efforts of NHS staff across England and I wish to place on record my appreciation for their engagement.
Richard Meddings, NHS England Chair.
Introduction from our chief executive
The NHS Operating Framework sets out our purpose to lead the NHS in England to deliver high-quality services for all. We must do that by supporting colleagues and leaders to deliver for patients, in what is a challenging context and environment.
The NHS Operating Framework also sets out our six longer-term aims that inform our near-term objectives. These aims are:
- Longer healthy life expectancy.
- Excellent quality, safety and outcomes.
- Excellent access and experience.
- Equity of healthy life expectancy, quality, safety, outcomes, access and experience.
- Value for taxpayers’ money.
- Support to society, the economy and environment.
In 2023/24 the NHS has three key tasks. The immediate priority is to recover our core services and productivity. Second, as we recover, we need to make progress in delivering the key ambitions in the NHS Long Term Plan . Third, we need to continue transforming the NHS for the future. Delivery of these three tasks depends on continuing to strengthen collaboration across the NHS and with partner organisations.
This business plan sets out NHS England’s work in leading and supporting the NHS to respond to these three key tasks. It also describes our fourth key task of completing the creation of our new organisation and continuing to improve how we work in line with our NHS Operating Framework.
This plan doesn’t describe everything we will do, but highlights our key commitments for 2023/24 under 12 headline objectives:
- Improve ambulance response and A&E waiting times.
- Reduce elective long waits and cancer backlogs and improve performance against the core diagnostic standard.
- Make it easier for people to access primary care services, particularly general practice.
- Improve mental health services and services for people with a learning disability and autistic people.
- Improve maternity and neonatal services.
- Prevent ill health and narrow health inequalities in access, outcomes, and experience.
- Recover productivity, increase efficiency and deliver a balanced financial position.
- Build and develop the workforce for now and the future.
- Build an improvement culture and drive improvements in quality.
- Transform care through harnessing data, information and technology.
- Change how we work, empowering and supporting local system partners to deliver on their responsibilities.
- Create a simpler, smaller, high-performing organisation through the New NHS England programme.
In delivering against these objectives, we will ensure that we continue to support the delivery of safe, high-quality care in everything we do, and meet the statutory duties of the new organisation.
The establishment of integrated care boards (ICBs) within integrated care systems (ICSs) and the new statutory framework means that NHS England is changing the way it works to best support and empower local system partners to deliver on their responsibilities. The Hewitt Review highlights the enormous promise of ICSs and the need to create the context within which they can thrive and deliver. We welcome the acknowledgement within the report of changes NHS England has already made to support system working, including:
- Coproduction and implementation of the NHS Operating Framework.
- Work to streamline and reduce the number of national priorities, as evidenced by a more focused 2023/24 Priorities and Operational Planning Guidance .
- Commitment to the co-development of national policy and strategy with ICB and ICS leaders.
We also recognise the need to go further and faster in some areas, giving system leaders the space, time and flexibility they need to deliver for their local communities, accompanied by robust accountability. We will use the Hewitt Review’s findings to inform our ongoing work to implement the new NHS England structures and NHS Operating Framework, as well as continuing to identify further opportunities to develop and implement ways of working that will support improvements to health outcomes, care quality, access and efficiency.
Amanda Pritchard , NHS Chief Executive.
Our plan on a page 2023/24

Our purpose: we are here to lead the NHS in England to deliver high quality services for all.
Our 6 longer term aims, also referred to as our ambitions: 1 longer healthy life expectancy, 2 excellent quality, safety and outcomes, 3 excellent access and experience, 4 equity of healthy life expectancy, quality, safety, outcomes, access and experience, 5 value for taxpayers money and 6 support to society, the economy and environment. We have 4 tasks for 2023/24.
Task 1. We must recover our core services and productivity by improving ambulance response and a and e waiting times; by reducing elective long waits and cancer backlogs and improving performance against the core diagnostics standard; by making it easier for people to access primary care services.
Task 2. We must make progress in delivering the key ambitions in the NHS Long Term Plan by improving mental health services and services for people with a learning disability and autistic people,; by improving maternity and neonatal services and by preventing ill health and narrow health inequalities in access, outcomes, and experience.
Task 3. We must continue transforming the NHS for the future by transforming care through harnessing data, information, technology and innovation.
Task 4. We will create the new NHS England and continue to change how we work by empowering and supporting local system partners to deliver on their responsibilities; by creating a simpler, smaller, high performing, organisation through the new NHS England programme.
Our final 3 objectives span all 4 tasks.
We will recover productivity, increase efficiency and deliver a balanced financial position.
We will build and develop the workforce for now and the future.
We will build an improvement culture and continue to drive improvements in quality.
1. Improve ambulance response and A&E waiting times
Urgent and emergency care services have been under growing pressure in recent years, and since the start of the pandemic have had to deal with a combination of issues affecting the flow of patients into, through and out of hospital.
The impact of these pressures is most visible in A&E performance, but also felt across the whole health and care system.
In January 2023, we published the Delivery plan for recovering urgent and emergency care services . That plan set out a range of measures to be taken by systems and providers to support recovery, with the key ambitions that:
- Patients should be seen more quickly in emergency departments: with the ambition to improve to 76% of patients being admitted, transferred or discharged within four hours by March 2024.
- Ambulances should get to patients who need them quicker: with improved ambulance response times for Category 2 incidents to 30 minutes on average over 2023/24.
Our priorities for 2023/24
- Increase capacity, to help deal with increasing pressures on hospitals.
- Grow the workforce, as increasing capacity requires more staff with the right skills, who feel supported and able to deliver the care patients need.
- Speed up discharge from hospitals, to free up more beds for those who need to be admitted.
- Expand and better join up health and care outside hospital, as up to 20% of emergency admissions can be avoided with the right care in place.
- Make it easier to access the right care, as 111 should be the first port of call and reduce the need for people to go to A&E.
We will also tackle unwarranted variation in performance in the most challenged local systems.
How we will deliver
Increase capacity.
- Provide dedicated funding of £1 billion to pay for additional capacity, including 5,000 new beds as part of the permanent bed base for next winter; and work with local areas to ensure that the new beds are put in place as sustainably as possible.
- Work with ambulance services and wider systems to increase capacity and ensure patients receive the most appropriate care, supported by dedicated additional funding of £200m.
- Provide £150 million to build 150 new facilities to support mental health urgent and emergency care services.
Grow the workforce
- Launch a new targeted campaign to encourage retired clinicians, and those nearing retirement, to work in 111 rather than leaving the NHS altogether.
- Make recruitment easier by reviewing the training and NHS Pathways licence requirements.
- Increase the number of emergency medical technicians to support the planned expansion of ambulance capacity.
Speed up discharge
- Continue to support implementation of the best practice interventions set out in the 100-day discharge challenge across NHS settings.
- Develop a new planning framework and national standard for rapid discharge into intermediate care, building on the learning from the frontrunner sites.
Make it easier to access the right care
- Provide national support and targeted funding to the continuing roll out of urgent community response (UCR) teams.
- Work with systems, building on the experience of ‘Getting it right first time’ (GIRFT), to establish a data-driven approach to peer review that supports implementation of new models of virtual wards.
- Roll out paediatric clinical assessment services to ensure specialist input for children and young people is embedded within 111.
- Work to integrate 111 online with the NHS App, and expand advice offered through NHS.UK and NHS 111 online .
- Undertake an extensive review of 111 services, including intensive trials of 111 First following lessons learnt in the 2019 pilot.
Reduce unwarranted variation by improving processes and standardising care
- Establish a new improvement programme, supported by national improvement collaboratives, to help standardise care.
- Set out priorities for local areas and acute providers in the delivery of acute frailty services and Same Day Emergency Care.
- Work with integrated care systems to fully embed year-round the system control centres.
2. Reduce elective long waits and cancer backlogs
As a direct consequence of the pandemic, many patients are waiting longer for the treatments they need. We are committed to delivering more planned hospital activity and improving performance for the longest waiting patients across elective care and cancer in line with the Delivery plan for tackling the COVID-19 backlog of elective care . We aim to ensure that by March 2024 no one waits longer than 65 weeks (except where patients choose to wait longer or in specific specialties).
Our national cancer awareness campaigns have successfully encouraged more people to come forward, resulting in a record number of urgent GP referrals. We have asked local systems to increase the percentage of cancers diagnosed at stages 1 and 2, meet the cancer faster diagnosis standard by March 2024, and continue to reduce the number of patients waiting over 62 days.
Timely access to diagnostics is critical to providing responsive, high-quality services and supporting elective recovery and early cancer diagnosis. We have asked local systems to deliver diagnostic activity levels that support plans to address elective and cancer backlogs as well as the diagnostic waiting time ambition (the ambition is that 95% of patients that receive a diagnostic test do so within six weeks by March 2025).
- Increase capacity and transform the way we provide elective care, to improve access and patient experience, and reduce long waits.
- Improve information and support for patients, to offer meaningful choice at the point of referral and at subsequent points in the pathway.
- Streamline cancer pathways and roll out targeted case-finding, to diagnose and treat cancer earlier and faster.
- Maximise the pace of roll-out of additional diagnostic capacity, to support the delivery of required diagnostic activity levels.
- Ensure the targeted investment fund (TIF) for elective recovery is committed to protecting and increasing elective activity.
- Develop and implement a new outpatient productivity programme that focuses on freeing up capacity to increase the number of first appointments for long waiters.
- Continue to develop patient-facing information on waiting times and how those on waiting lists can help manage their condition through My Planned Care .
- Target improvement/transformation support to the most challenged providers, and clinical specialty pathways.
- Develop a Patient Initiated Digital Mutual Aid System (PIDMAS) which will offer patients the ability to opt-in to move provider when they have been waiting over 40 weeks for care.
- Provide over £390m in cancer service development funding to cancer alliances to support delivery of early diagnosis and key operational priorities.
- Continue the rollout of non-specific symptoms pathways.
- Support the rollout of targeted lung health check sites and increase capacity through investment in computerised tomography scanner capacity.
Diagnostics
- Provide funding to support the development of pathology and imaging networks and the development and rollout of community diagnostic centres (CDCs) (£2.3bn of capital funding to 2025 has also been allocated to support diagnostic service transformation, including to implement CDCs, endoscopy, imaging equipment and digital diagnostics).
- Support the rollout of CDCs and associated workforce growth to increase diagnostic pathway capacity.
- Support the development of diagnostic networks and digital diagnostics infrastructure.
- Work with systems to improve service utilisation, productivity and patient throughput.
3. Make it easier for people to access primary care services, particularly general practice
GPs and their growing teams continue to deliver more appointments for patients; in the 2022/23 financial year they provided an average of 28 million appointments every month, 1.3 million more than in 2021/22. More than two thirds of appointments are face-to-face, and more than half are held on the same day as booking, or the day after.
However, demand for appointments remains high, and many patients report issues with contacting their practice or securing appointments when they want them.
In May 2023, we published our Delivery plan for recovering access to primary care , which set out our ambitions to tackle the 8am rush and make it easier and quicker for patients to get the help they need from primary care. The plan sets out how we will do this by:
- Empowering patients, so they can more effectively manage their own health.
- Implementing modern general practice access , so patients know on the day how their request will be handled.
- Building capacity , so practices can offer more appointments from more staff than ever before.
- Cutting bureaucracy , to give practice teams more time to focus on their patients’ clinical needs.
ICBs are accountable to NHS England for the commissioning of general practice services and delivery against the contract. From April 2023, all ICBs have accountability for commissioning community pharmacy, dental and optometry services. NHS England will ask and support ICBs to develop their own system level access improvement plan.
Empowering patients
- Improve information and NHS App functionality, so that patients registered with over 90% of practices have access to health information they can trust and can manage routine appointments.
- Expand community pharmacy services, to give people easy access to more health services in the heart of their communities.
Implementing modern general practice access
- Transition practices to digital telephony, so patients get a better experience when they call their practice.
- Simplify online requests and improve care navigation, to make it easier for people to contact their practice and to make getting a response the same day standard procedure.
Building capacity
- Continue to support the growth of larger multidisciplinary teams, to optimise the use of the full practice team and help manage more patient requests.
- Continue to support the recruitment and retention of doctors in general practice, to address the gap between capacity and demand.
- Transform the NHS App to support the ambition for 75% of all adults in England to be registered on the NHS App by March 2024.
- Expand the information available through NHS.uk on local services and improve the existing monitoring tools.
- Launch Pharmacy First (subject to a DHSC led consultation with Pharmaceutical Services Negotiating Committee) enabling pharmacists to supply prescription-only medicines to treat common health conditions where clinically appropriate.
- Improve the digital infrastructure between general practice and community pharmacy to streamline referrals.
- Support the transition to digital telephony (for practices that commit by 1 July 2023 to the move), including procurement, contract negotiation and financial support for new equipment, buy out costs and training.
- Make high quality online consultation, messaging and booking tools available to general practice, alongside guidance on the relative strengths of the tools in different areas.
- Invest in a new National Care Navigation Training Programme for up to 6,500 staff.
- Continue to provide systems with £4 million of System Development Funding (SDF) which they can use to recruit and retain general practice nurses, and make up to a further £385 million available in Additional Roles Reimbursement Scheme (ARRS) funding to continue to grow capacity.
- Publish guidance, developed with frontline staff, to help practices make best use of ARRS roles.
- Work with partners to facilitate ways in which doctors other than GPs can work in general practice as part of a multidisciplinary team to help increase practice capacity.
- Continue to invest in GP retention schemes and run a campaign to encourage GPs to return to general practice or to support NHS 111.
From May 2023, NHS England will introduce a National General Practice Improvement Programme with three tiers of support to help general practice deliver change.
We will also develop and begin to implement dental reform proposals targeted at improving access, provision, workforce and prevention.
4. Improve mental health services and services for people with a learning disability and autistic people
The COVID-19 pandemic has had a significant impact on the physical and mental health of people with a learning disability and autistic people, and increased the prevalence, acuity and complexity of mental health needs.
We have asked local systems to continue to focus on delivering our core NHS Long Term Plan commitments to improve mental health services and services for people with a learning disability and autistic people.
- Expand access to NHS Talking Therapies, and children and young people’s (CYP), community, and perinatal mental health services.
- Drive quality of services through transformation of models of care.
- Support the recovery of the Urgent and Emergency Care pathway.
- Improve the physical and mental health of people with a learning disability and autistic people.
- Improve the quality and reduce the reliance on inpatient care for people with a learning disability and/or autistic people.
Mental health
- Promote the rebrand of NHS Talking Therapies to increase access to services.
- Expand the roll out of mental health support teams in schools and support systems to increase access to perinatal and maternal mental health services.
- Publish updated guidance for the Children and Young People Eating Disorder Standards, Crisis provision and dementia diagnosis patient pathways.
- Support the delivery of new models of community mental health services integrated with primary care.
- Work across all systems to support demand and capacity management in light of increased prevalence.
- Create a strategy for integrating digital health technologies in mental health settings and pathways.
- Support the development of new and expanded roles, such as peer support workers and allied health professionals in mental health to increase the size of the mental health workforce.

Learning disability and autism
- Publish best practice toolkits/guidance to improve uptake of learning disability annual health checks and improve the quality and access to health and social care for autistic people.
- Publish guidance and design and implement a support offer for systems to deliver the Localising Care Commitment.
- Support implementation of the Dynamic Support Register and Care, Education, and Treatment Review.
5. Improve maternity and neonatal services
In March 2023 we published the Three year delivery plan for maternity and neonatal services . The plan sets out how the NHS will make care safer, more personalised, and more equitable. This consolidates the improvement actions committed to in Better Births, the NHS Long Term Plan, the Neonatal Critical Care Review, and reports of the independent investigation at Shrewsbury and Telford Hospital NHS Trust and the independent investigation into maternity and neonatal services in East Kent.
- Improve equity for mothers and babies and deliver care that is personalised.
- Retain, grow and invest in our workforce.
- Support a culture of safety, learning, and support.
- Support the implementation of best practice and use of data.
Equity and personalised care
- Pilot and evaluate new service models designed to reduce inequalities, including enhanced midwifery continuity of carer.
- Publish national postnatal care guidance, setting out the fundamental components of high-quality postnatal care.
- Publish a national service specification and implementation guidance for perinatal pelvic health services.
- Act on findings from the evaluation of independent senior advocate pilots as set out in the interim Ockenden report.
- Invest to ensure the availability of bereavement services seven days a week.
Retain, grow and invest in our workforce
- Fund a retention midwife in every maternity unit during 2023/24.
- Strengthen neonatal clinical leadership with a national clinical director for neonatal and national neonatal nurse lead.
- Provide funding to establish neonatal nurse quality and governance roles within trusts.
- Assist trusts with their workforce plans by providing direct support, including through operational delivery networks for neonatal staffing.
- Work with the Royal College of Obstetricians and Gynaecologists to develop leadership role descriptors for obstetricians to support job planning, leadership and development.
- Provide tools to support implementation of the maternity support worker competency, education, and career development framework.
Culture of safety, learning, and support
- Offer the perinatal culture and leadership programme to all maternity and neonatal leadership quadrumvirates.
- Support the transition to the patient safety incident response framework through national learning events patient safety incident response framework.
- Provide nationally consistent support for trusts that need it through the Maternity Safety Support programme.
- Support trust board assurance, oversight of maternity and neonatal services through delivery of the maternity and neonatal board safety champions programme.
Best practice and data
- Keep best practice up to date through version 3 of the Saving Babies Lives Care Bundle.
- Convene a taskforce to progress the recommendation from the Kirkup report for an early warning system to detect safety issues within maternity and neonatal services.
6. Prevent ill health and tackle health inequalities
Prevention is a crucial part of the NHS’s approach to improving overall population health and reducing health inequalities, helping people to make healthier lifestyle choices and treating illness at an early stage, so they can live longer, healthier lives. In 2023/24 we will continue to support the delivery of evidence-based NHS prevention programmes to optimise care for cardiovascular disease (CVD) and diabetes, and reduce smoking, obesity and alcohol intake.
Under the agreement made between the Secretary of State and NHS England under section 7A of the National Health Service Act 2006, we are responsible for the commissioning of national screening and immunisation programmes, including those for bowel and breast cancer, cervical screening, childhood immunisations and the influenza vaccination. In 2023/24, we will continue to work to expand eligibility, improve the detection of cancers and implement plans to address health inequalities in uptake.
The COVID-19 pandemic has highlighted and exacerbated existing health inequalities, with its disproportionate impact on people and communities already at highest risk. In 2023/24, we will continue to support the NHS to realise the ambition of reducing healthcare inequalities through equitable access, excellent experience and optimal outcomes for all.
- Support improved clinical management of cardiovascular disease, respiratory disease and diabetes, to prevent avoidable ill-health and reduce health inequalities.
- Optimise the impact of healthcare on the population through the prevention of ill health, enabling longer healthier lives for all.
- Increase uptake and coverage in vaccination and screening, reducing unwarranted variation and disparities.
- Support delivery of the NHS’s five strategic priorities for tackling healthcare inequalities (they are (1) restore NHS services inclusively; (2) mitigate against digital exclusion; (3) ensure datasets are complete and timely; (4) accelerate preventative programmes; (4) strengthen leadership and accountability), to reduce unfair and avoidable differences in health across the population.
Major conditions and public health
- Develop cardiac and pulmonary rehabilitation resources to support local decision making and improve access.
- Complete a secondary prevention review with systems and publish evidence and resources to support local decision making.
- Deliver national services to support improvements in Type 2 diabetes prevention and remission services and national digital structured education support for Type 1 and Type 2 diabetes.
- Develop a digital tobacco dependency service and begin to implement it, with an initial focus on NHS staff.
- Provide support to key NHS England programmes to maximise their health impact, with a focus on health and care inequalities and improving healthy life expectancy.
Screening and vaccinations
- Develop and publish a vaccination strategy and start implementation in partnership with regional teams and ICSs.
- Develop strategies for NHS screening and Child Health Information Services (CHIS) and develop a plan for potential future delegation of elements of screening commissioning to ICBs.
- Enhance the vaccinations digital platform, developing a national vaccination record, extending the use of the NHS App and establishing the foundations for a lower cost base.
- Implement the digital transformation of screening, to deliver new digital products for the invitation of, and communication with, eligible members of the public for the breast and diabetic eye programmes.
Health inequalities
- a healthcare inequalities strategy, with supporting resources including a new system accountability framework and framework for NHS action on inclusion health
- an updated Healthcare Inequalities Improvement Dashboard with a new measurement framework and indicators to support improvement and drive local accountability
- a framework to support focused NHS action on digital inclusion and develop a two-year implementation plan
- a handbook to support Core20PLUS5 implementation.
- Fund the recruitment of 350 connector roles (connectors are those with influence in their community who can help engage local people with health services, including vaccine champions, peer advocates and social prescribing link workers) to support Core20PLUS5 implementation.
- Support the continued roll out of High Intensity User services.
7. Recover productivity, increase efficiency and deliver a balanced financial position
NHS England’s revenue and capital resource limits for 2023 to 2024 are published in the 2023 to 2024 Financial Directions to NHS England . The Government expects NHS England to ensure that overall financial balance is delivered for the NHS every year.
To deliver a balanced net system financial position for 2023/24 and achieve our core service recovery objectives, we must meet the 2.2% efficiency target agreed with government and improve levels of productivity. Most of this will need to be delivered via local ICBs and provider organisations. Local systems will be supported in this by a national efficiency programme that reports into the National Productivity Board.
- Support ICSs to transform care pathways and embed continuous improvement (see objective 9)
- Support NHS providers to reduce their agency staff bills and encourage workers back into substantive and bank roles.
- Drive efficiencies from the NHS’s investment in medicines.
- Drive commercial excellence and efficiencies in NHS procurement and corporate running costs.
- Improve NHS estates productivity and efficiency.
- Provide the NHS with access to near real-time data to support the identification of barriers to improved productivity delivery.
- Address unwarranted variation across clinical pathways through delivery of the GIRFT programme.
- Develop a workforce productivity diagnostic tool to support the identification of service level productivity gaps.
- Develop, negotiate and implement a new Voluntary scheme for branded medicines pricing and access (VPAS) framework to secure value for money of overall branded medicines expenditure.
- Deliver a medicines efficiency programme to maximise value from medicines procurement.
- Deliver a commercial efficiency programme to maximise value from non-clinical NHS procurement.
- Create system wide strategies for priority non-pay spend categories to support innovation and deliver efficiencies.
- Support the development of robotic process automation and other technologies that reduce the transactional administrative burden on the NHS.
- Support delivery of a capital programme across the NHS estate, improve long term planning and drive savings through a reduction in non-clinical space.
8. Build and develop the workforce for now and the future
The NHS workforce is at the heart of providing high quality patient care, and investment in staff is key to delivering the improvements in services needed for patients.
In July 2023 we published our NHS Long Term Workforce Plan , which includes independently verified forecasts for the number of doctors, nurses and other professionals that will be needed in 5, 10 and 15 years’ time, taking full account of improvements in retention and productivity, and details the actions that will be taken to train, retain and reform the NHS workforce.
- Recruit more staff, domestically and internationally, to respond to local needs and reduce NHS vacancy rates.
- Increase the number of qualified healthcare professionals, through quality education and training, reflecting local need.
- Review and reform education and training , to better meet patient and student needs.
- Support the use of digital technology, innovation and workforce transformation, to help increase the time to care and respond to changing population needs.
- Improve NHS leadership, talent and management practices.
- Improve staff retention and experience and ensure equality, diversity and inclusion for all staff.
- Support expansion of the workforce and development of new roles aligned to key service development priorities.
- Implement the global health workforce strategy.
- Deliver the 2023/24 METIP (Multi-Professional Education and Training Investment Plan, the annual investment planning process developed by Health Education England) plan for medics, and clinical professions and develop the Clinical Placement Management System.
- Develop and deliver an implementation plan to accompany the new Educator Workforce Strategy to create a sustainable supply of clinical educators.
- Develop more flexible routes into training such as apprenticeships that will help to grow and diversify the talent pool.
- Improve the quality of healthcare education and training and reduce course leaving rates.
- Expand trailblazer learner cohorts to enhance the generalist skills of postgraduate doctors.
- Increase the number of adult nurse and midwife students on blended learning degrees.
- Develop plans to improve the medical education and pharmacy training programmes.
- Develop a national learning hub to promote the growth of our educational resources and learning opportunities.
- Develop and roll out digital solutions (staff app, digital staff passport) to support flexible working practices and flexible deployment of staff across organisational boundaries.
- Maximise opportunities for new ways of working by upskilling, enhanced, advanced and consultant practice.
- Co-produce management, talent and leadership development products, taking account of the Messenger review.
- Develop and support implementation of interventions to deliver on the People Promise, improving staff experience and retention.
- Provide leadership and interventions to improve health and wellbeing.
- Implement the Kark recommendations and the Fit and Proper Persons test.
- Publish and support implementation of a five-year NHS Equality Diversity and Inclusion Improvement Plan.
- Implement national and regional Workforce Race Equality Standard (WRES) and Workforce Disability Equality Standard (WDES) action plans.
- Provide leadership in developing the future of NHS HR and OD and support capability building.
9. Build an improvement culture and continue to drive improvements in quality
In April 2023, we published the findings of the NHS delivery and continuous improvement review , which explores how the NHS can develop a culture for continuous improvement while focusing on its most pressing priorities. We will take the actions from the review forward as part of our wider programme to support improvements in care quality and outcomes.
- Support the development of capacity and capability, to continuously improve quality and transform care.
- Deliver improvement and transformation, across whole pathways.
- Support ICSs to manage and improve the quality of their services, and deliver their statutory quality duties.
- Support the ongoing implementation of the Patient Safety Strategy and delivery of patient safety statutory duties.
- Establish a National Improvement Board to support the implementation of improvement approaches across the NHS.
- Continue to establish NHS Impact – Improving Patient Care Together – as a shared approach to purposeful improvement across the NHS.
- Support providers and systems to develop the leadership behaviours, culture, capability, capacity and management systems to use a comprehensive approach to continuous quality improvement to address variation in performance, productivity, quality and staff experience.
- Develop a strategy for NHS England’s clinical effectiveness programmes to improve patient outcomes and increase the impact of clinical effectiveness information.
- Deliver improvement across care pathways and reduce unwarranted variation through the GIRFT programme, the Outcomes and Registries programme, national clinical audits and the National Consultation Information Portal.
- Deliver the radiotherapy transformation programme through networks and cancer alliances.
- Publish and implement an Operating Model for Quality, working with systems, regulators and other partners.
- Provide guidance, best practice and peer support to ICSs to manage the quality of services, and support delivery of their statutory quality duties.
- Pilot System Quality Accounts to support improvement of care quality through ICSs.
- Embed the quality framework across all specialised service governance and programmes.
- Lead transformation of how the NHS responds to patient safety incidents by implementing the new Patient Safety Incident Response Framework (PSIRF), with all secondary care providers transitioned.
- Replace the legacy National Reporting and Learning System with the new Learn from patient safety events (LFPSE) service, supporting all providers to transition to the new system.
- Launch training in levels 3 and 4 of the Patient Safety Syllabus for all patient safety specialists in the NHS.
10. Transform care through harnessing data, information and technology
The merger of NHS England with NHS Digital from 1 February 2023 provides us with the opportunity to accelerate the digitally enabled transformation of the NHS, adopting effective technologies and building on insights from data and cutting-edge research.
NHS England will continue to work with systems to level up digital infrastructure, drive greater connectivity and support the development of a digital first option for the public, helping patients identify their needs, manage their health, and get the right care in the right setting. Our work will focus on three areas:
- Digitise, ensuring that digital foundations are in place everywhere.
- Connect , helping the different parts of the NHS to work together through improved useability, connectivity and interoperability.
- Transform, using digital products and leveraging innovation and research to transform health and care.
- Ensure that 90% of trusts have an electronic patient record (EPR).
- Deliver technology upgrades across primary care, widen access to GP record data, and support delivery of the Primary Care Access Recovery Plan.
- Continue to develop a portfolio of core digital products and services, to support improved outcomes and address legacy technology constraints.
- Develop the NHS App as the digital front door of the NHS.
- Accelerate the uptake of the most promising Artificial Intelligence (AI) technologies.
- Extend access to molecular diagnostics and genomic testing, to over 100,000 patients newly diagnosed with cancer.
- Develop and deploy a support offer to trusts undertaking EPR-related transformation and publish Minimum Digital Foundations guidance.
- Provide practices with the digital tools to support Modern General Practice Access, and fund transition cover (for those that commit to adopt this approach before March 2025).
- Procure a Federated Data Platform, available to all ICSs, with nationally developed functionality including tools to help maximise capacity, reduce waiting lists, and coordinate care.
- Ensure healthcare professionals can view, access and import a patient’s full GP clinical record irrespective of their care setting or organisation.
- Accelerate the ambition of reducing the reporting burden on providers and addressing the need for more timely automated data, so that all acute NHS trusts are using Faster Data Flows.
- Deliver new functionality for the NHS App, to help people take greater control over their health and their interactions with the NHS.
- Pilot an Artificial Intelligence deployment platform.
- Support rapid cancer genomics through the Genomic Pathology Accelerator Programme.
We will also support local NHS and social care organisations to manage cyber risk and ensure compliance with national cyber standards in each ICS and NHS region.
11. Change how we work, empowering and supporting local system partners to deliver on their responsibilities
The establishment of ICSs and the new statutory framework means that NHS England is changing the way it works (our operating framework) to best empower and support local system partners to deliver on their responsibilities. This requires a cultural and behavioural shift towards partnership-based working; creating NHS policy, strategy, priorities and delivery solutions with national partners and with system stakeholders; and giving system leaders the agency and autonomy to identify the best way to deliver agreed priorities in their local context.
We will support local decision making, empowering local leaders to make the best decisions for their local populations and focus on what we are uniquely placed to do as a national organisation, increasingly using our resources to provide practical support to colleagues within systems.
- Embed the ways of working and leadership behaviours set out in the NHS Operating Framework, to best empower and support local system partners to deliver on their responsibilities.
- Set national direction, strategy and evidence-based policy, to support the continued development of ICSs.
- Support the development of mature, collaborative ways of working within ICSs at system, place and provider level, to create the environment for sustainable, ongoing peer-led system development.
- Complete the successful transfer of new delegations from NHS England to ICSs, to enable local systems to design and deliver more joined-up care for their patients and communities.
- Design, test and implement a new approach to the co-production of strategy and policy with systems and national partners.
- Update the NHS Oversight Framework and work with ICBs to ensure oversight and performance management arrangements within their ICS area are proportionate and streamlined.
- Agree a wider accountability framework for ICSs with DHSC, CQC and other national partners.
- Deliver the second phase of the Place Development Programme, supporting systems to design and test new integrated ‘at scale’ care models.
- Deliver the provider collaboratives innovator scheme and publish updated guidance to help accelerate the development of collaboratives.
- Implement statutory joint committees of ICBs and NHS England to oversee commissioning of appropriate specialised services across multi-ICB populations ahead of ICBs taking on this delegated responsibility in April 2024.
- Provide ICBs with tools and resources to support transformation, and to further develop their understanding of specialised services and enable them to realise the benefits of integration.
12. Create a simpler, smaller, high performing organisation through the new NHS England programme
The creation of ICSs; the merger of NHS England, with NHS Digital on 1 February 2023, and Health Education England on 1 April 2023; and the need to resize our organisation following the Covid-19 pandemic mean we must create a new NHS England. Our aim is to create a simpler, smaller, high performing, organisation that leads the NHS more effectively and is a better place to work. We will be more joined up and efficient, speaking with one voice to the service.
We expect that, by April 2024, our new single organisation will be at least 30%, and up to 40%, smaller than the previous combined size of NHS England, Health Education England and NHS Digital.
- Design the new NHS England, including how we will organise ourselves to deliver the new organisation’s priorities.
- Complete the successful implementation of the new staffing structure, including the transfer of NHS England staff working in the delegated NHS England commissioning functions.
- Complete all merger-related activities, including the harmonisation of policy, process, and corporate functions and infrastructure across the new organisation.
- Shape our new culture, to make NHS England a great place to work for our people and help us achieve our inclusion, diversity and wellbeing ambitions.
- Continue to develop and implement our operating framework.
- Complete staff consultations and the process for filling of posts.
- Deliver a full set of harmonised corporate policies.
- Develop a new Risk Management Framework including operational and clinical risk management.
- Establish appropriate data safe haven processes and governance in line with statutory requirements and guidance.
- Develop and implement a culture change plan.
Our funding
Our commissioning budget for 2023/24 is £168.8 billion. We are responsible for using this money wisely, fairly and transparently to secure the best possible outcomes for both patients and the taxpayer.
We allocate most of this funding – £114.3 billion – to integrated care boards for commissioning local health services. A further £32.3 billion is spent on directly commissioning services including some primary care services, specialised services and public health. £4.9 billion is spent on educating and training the health workforce through an annual investment planning process called the Multi-Professional Education and Training Investment Plan (METIP). The remaining funds are allocated to the delivery of service development and improvement programmes, in line with our corporate priorities (the large majority of the Service Development Fund and Elective Recovery Fund is allocated directly to ICBs for commissioning local health services), and NHS England’s core administration and programme costs. Figure 1 shows how we distribute our mandate funding.
Figure 1: 2023/24 NHS England mandate revenue funding (£168.8 billion)
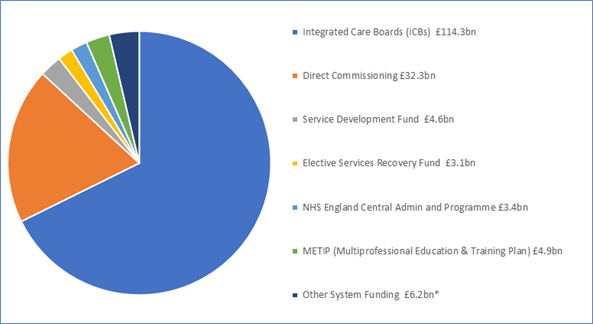
* ‘Other System Funding’ includes £3.6bn for increased employer pension contributions.
Image alternative text: Integrated Care Boards £114.3 billion. Direct Commissioning £32.3 billion. Service development fund £4.6 billion. Elective services recovery fund £3.1 billion. NHS England central admin and programme £3.4 billion. Multi-professional education and training plan £4.9 billion. Other system funding £6.2 billion, including £3.6 billion for increased employer pension contributions.
Our programme costs are focused on the delivery of our corporate priorities and this year we have a funding envelope of £2.3 billion. The central administration budget for NHS England in 2023/24 has been set at £0.7 billion.
Figure 2: 2023/24 NHS England central admin and programme revenue funding (£3.4 billion)
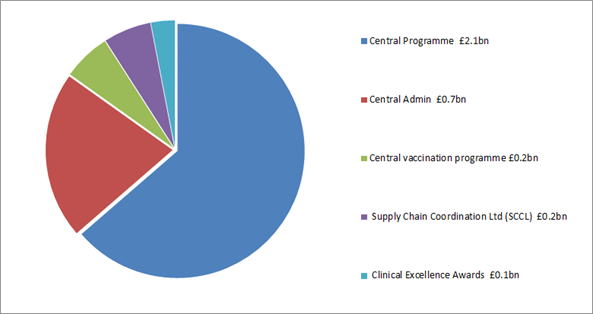
Image alternative text: Integrated Care Boards £114.3 billion. Direct Commissioning £32.3 billion. Service development fund £4.6 billion. Elective services recovery fund £3.1 billion. NHS England central admin and programme £3.4 billion. Multi-professional education and training plan £4.9 billion. Other system funding £6.2 billion, including £3.6 billion for increased employer pension contributions
Publication reference: PRN00201

IMAGES